Researchers at The University of Texas MD Anderson Cancer Center have discovered that two distinct classes of cancer-associated fibroblasts (CAFs) accumulate in the pancreatic tumor microenvironment and play opposing roles to promote and restrain pancreatic cancer development. The combined results of human pancreatic tumor analyses, and experiments in mouse models, suggest that appropriately targeting these unique CAF populations may offer strategies to improve the use of other treatments, such as chemotherapy and immunotherapy.
“Cancer-associated fibroblasts are known to regulate cancer progression, but targeting these cells in pancreatic cancer has largely failed to improve patient outcomes and has, in some cases, worsened response,” said lead author Kathleen McAndrews, PhD, postdoctoral fellow in Cancer Biology. “Our findings provide the first evidence of the functional heterogeneity of CAFs in pancreatic cancer that may explain the variations in patient outcomes.”
McAndrews and colleagues published their study results in Cancer Discovery, in a paper titled “Identification of Functional Heterogeneity of Carcinoma-Associated Fibroblasts with Distinct IL-6 Mediated Therapy Resistance in Pancreatic Cancer.”
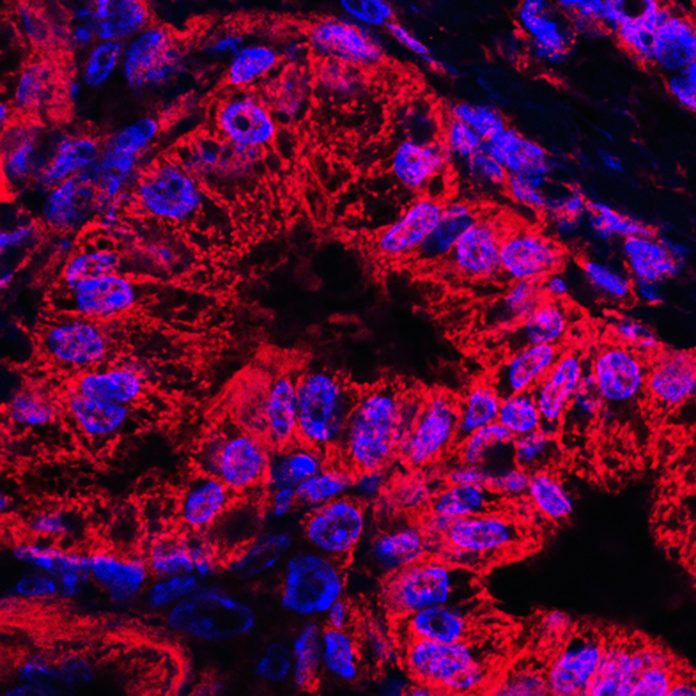
Fibroblasts, a type of cell found in connective tissue, are involved in important biological processes, such as wound repair. Cancer-associated fibroblasts accumulate in tumors, and can be found in large numbers in pancreatic cancers. “The tumor microenvironment in pancreatic ductal adenocarcinoma (PDAC) involves a significant accumulation of fibroblasts as part of the host response to cancer,” the authors wrote. “The focus on CAFs in pancreatic cancer has been driven by the fact that, in some patients, stromal cells (including fibroblasts) can out-number the cancer cells … However, the precise role of CAFs in PDAC progression remains unknown.”
Interestingly, in their newly reported studies, McAndrews and colleagues found that expression of these proteins in treatment-naïve human tumor samples correlated with patient outcomes. Increased expression of αSMA was associated with significantly improved overall survival (OS), whereas elevated FAP levels were associated with significantly decreased OS.For their studies, the researchers performed single-cell RNA sequencing (scRNA-seq) to analyze gene expression and clarify the types of CAFs present in pancreatic tumors. They focused on two distinct subsets of CAFs marked by expression of fibroblast activation protein (FAP) and alpha-smooth muscle actin (αSMA). Previous work had indicated that FAP-expressing CAFs could promote PDAC tumor growth, the authors pointed out, and “Recent studies have suggested that targeting FAP+ CAFs may lead to suppression of tumor growth.” In contrast, they noted, “Previous studies showed that the overall functional contribution of αSMA+ CAFs is tumor restraining.”
Using novel mouse models, the researchers next demonstrated that FAP+ and αSMA+ CAFs play distinct and opposing roles in the tumor microenvironment. Loss of FAP+ cells suppressed tumor progression and improved OS, suggesting that these cells act to promote tumor development. Conversely, loss of αSMA+ fibroblasts resulted in more aggressive tumors and shorter OS, indicating that these cells work to block pancreatic cancer progression.
Loss of FAP+ vs. αSMA+ cells was associated with distinct gene expression changes in the tumor, resulting in altered regulation of various cancer-associated pathways and different accumulation of immune cells in the tumor microenvironment. “Interestingly, FAP+ CAF depletion was associated with upregulation of largely distinct pathways related to protein processing, proteolysis, fibrinogen and blood coagulation, cell junctions, endopeptidase inhibitor activity, and pancreatic secretion, potentially reflecting the improved histology in FAP+ CAF-depleted tumors,” they reported. “In αSMA+ CAF-depleted tumors, gene expression changes were associated with pathways related to epithelial migration, cell proliferation, cytokine production, inflammatory responses, as well as T and B cell-related immunity.”
To clarify the distinct roles of FAP+ and αSMA+ cells, the research team analyzed secreted proteins that may affect the tumor and surrounding cells. The immune signaling protein interleukin 6 (IL-6) is produced by both classes of CAFs. Loss of IL-6 in αSMA+ cells, but not FAP+ cells, improved responses to chemotherapy and immunotherapy with significantly improved OS. “Our study reveals the complexity of CAF biology in PDAC, specifically the different CAF roles in natural progression of the disease and how their function(s) impacts therapeutic intervention,” the authors noted.
The results highlight the heterogeneous roles of these different classes of CAFs, explained senior author Raghu Kalluri, MD, PhD, professor and chair of Cancer Biology. “This is a new discovery that helps move the field forward, with a new appreciation of the biology of pancreatic cancer and possible strategies for therapeutic interventions,” Kalluri said. “Our next steps are to identify therapies that can target the tumor promoting fibroblasts while sparing the sum beneficial responses of our body in its effort to fight cancer.”
The authors further concluded, “collectively our studies show that targeting FAP+ CAFs emerges as a viable strategy to achieve inhibition of PDAC.” They suggested that FAP directed-CAR T cell therapy might be one effective strategy, which has previously been demonstrated. “Targeting chemokines that are selectively secreted by FAP+ CAFs might be a viable strategy also,” they noted. “Strategies to increase the number of SMA+ CAFs can represent another strategy to control PDAC.”













