Researchers at the University of British Columbia (UBC), BC Cancer, Harvard Medical School, and Memorial Sloan Kettering Cancer Center (MSK) have identified early genetic alterations in healthy women’s breast cells that could be among the first steps leading to breast cancer. The findings, published today in Nature Genetics, suggest that cancer-like mutations appear silently in breast cells that appear normal, potentially offering insights into the origins of the disease.
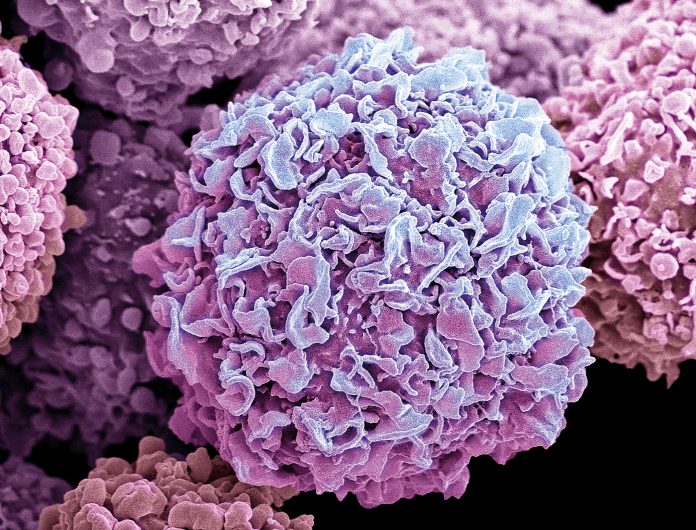
The study analyzed the genomes of more than 48,000 individual breast cells from women without breast cancer, using an advanced single-cell sequencing technique called DLP+, a method for high-throughput single-cell DNA sequencing that combines automation, a powerful microscope, robust DNA sequencing chemistry, and computational software to provide an unprecedented level of resolution to the understanding of tumor evolution.
The researchers found that while the majority of cells appeared healthy, nearly all of the women in the study harbored a small number of cells—about three percent—that carried genetic alterations typically associated with cancer. These mutations, known as copy number alterations (CNAs), involve the duplication or loss of large segments of DNA.
“It’s striking to see cancer-like mutations happening silently and at low levels in the cells of perfectly healthy women,” said lead senior study author Samuel Aparicio, PhD, a professor at UBC’s Faculty of Medicine and a distinguished scientist at BC Cancer. “While harmless on their own, these changes could be the basic building blocks of breast cancer. With further research into how these mutations arise and accumulate, we could potentially develop new and lifesaving preventive strategies, therapeutic approaches, and routes for early detection.”
CNAs, are alterations in the structure of chromosomes, which are usually corrected by the body’s natural DNA repair mechanisms. However, if these repair processes fail, the mutations can accumulate, eventually leading to cancer. The study’s primary goal was to explore the prevalence of CNAs in breast cells from women without cancer. The researchers focused on two main types of cells in the breast: luminal cells, which line the ducts and lobules where milk flows, and contractile cells. While genetic changes were found in both cell types, they were far more common in the luminal cells.
“Since luminal cells are believed to be the cells of origin of all of the major types of breast cancer, the fact that these genetic alterations specifically accumulate in luminal cells provides additional support for the hypothesis that these alterations may prime or predispose these cells to cancer development,” said Joan Brugge, a co-senior author of the study and a professor of cell biology at Harvard Medical School. “This study is an important step on our collective quest as scientists to understand the earliest events in breast cancer development. These insights can inform our efforts to design new, more effective prevention and monitoring strategies for those at high risk for cancer.”
The study also found that while the majority of cells contained only one or two CNAs, in some women who carried germline BRCA1 and BRCA2 high-risk variants, that there a number of “extreme” examples of cells having six or more of these large genetic changes.
“To study this phenomenon, we used a method originally developed to study genome instability in cancer, providing a comprehensive view of copy number alterations at the single-cell level,” said Sohrab Shah, PhD, chief of computational oncology at MSK. “Our computational approaches further allowed us to identify and analyze these rare events that are not visible with standard sequencing assays.”
The implications of these findings are significant, as they raise new questions about the processes that lead to breast cancer. For example, why do mutations only occur in luminal cells, and how do these mutations accumulate over time? The researchers also noted that the presence of these alterations in normal tissue could be a sign of a potential progression pathway from healthy to cancerous cells. The next steps for researchers include studying how these mutations evolve and what factors may influence their development.
“We speculate that the CNA mutational events that accumulate later in the progression from normal epithelium to cancer may be dependent on these earlier alterations,” the researchers wrote. “For example, it is known that MYC overexpression sensitizes cells to apoptosis, and survival of high MYC cells requires anti-apoptotic alterations like p53 loss of function or gain of BCL2 anti-apoptotic proteins.”
Further study is needed to determine whether these early genetic changes could be targeted for prevention or early detection of breast cancer. The discovery also suggests the potential to identify at-risk individuals based on the presence of these mutations. The patterns of genetic alterations found in this study are consistent with those seen in low-grade breast cancers, suggesting that these mutations may be among the earliest events in cancer development.













