Researchers at the Gladstone Institutes have developed a CRISPR-based “genome shredding” technique that shows promise in treating glioblastoma, an incurable brain cancer. Their research was published this week in the journal Cell Reports.
Much of the work done to develop the technique was done in the lab of Jennifer Doudna, PhD, an author on the paper, and co-winner of the 2020 Nobel Prize in Chemistry for the discovery of CRISPR-Cas9 gene editing technology. Other key players are Mitchel Berger, MD, a neurosurgeon and director of the Brain Tumor Center at University of California, San Francisco (UCSF), whose team helped secure patient-derived cell samples, and Alexendar Perez, MD, PhD, a resident at UCSF who performed much of the computational analysis needed for the study.
Computational analysis was necessary for diving into the non-coding portions of the genome to identify repetitive sequences shared by the glioblastoma cells. Cancer treatments rarely kill all tumor cells. In glioblastoma and other highly recurrent cancers, tumor cells that escape treatment develop multiple genetic mutations that allow them to proliferate.
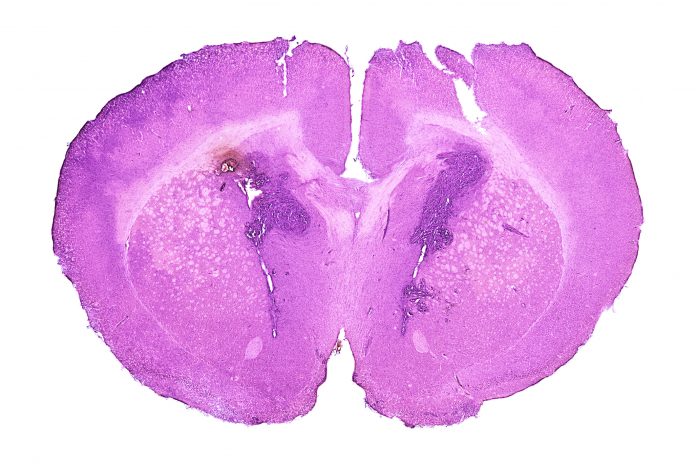
Building on prior research, the Gladstone team surmised that mutated glioblastoma cells have a unique genetic signature that could be targeted. According to the paper, the team identified “unique recurrent GBM-specific sgRNAs” mainly in the non-coding genome that were “generated by TMZ [chemotherapy] signature mutations characteristic of hypermutated gliomas.” Those sequences are the beacon that guides CRISPR to the cancerous cells where it cuts up them up “leading to genome fragmentation and DNA damage-induced cell death.”
There is a lot to do before this CRISPR-based genome shredding technique can be used therapeutically. For example, the researchers noted that there are inefficiencies in the delivery modalities that need to be addressed. And it is important to note that the work published in Cell Reports does not detail a path to direct clinical implementation for this approach. But the results are promising evidence of CRISPR’s potential to treat not just glioblastoma but other hypermutated tumors, according to Christof Fellmann, PhD, study lead and corresponding author on the paper. “We see CRISPR as a gateway to a new therapeutic approach that won’t be subject to the possibility of tumor cell escape.”
And the researchers have reason to be hopeful. Results in the paper indicate that the technique works only on the tumor cells, sparing healthy ones during treatment. And in cases where tumor cells escaped the initial shredding, they succumbed to a second round of treatment. “We understand so much today about glioblastoma and its biology, yet the treatment regimens haven’t improved,” said I-Li Tan, PhD, first author on the paper. “Now we have a precise way to target the cells that are driving the cancer, and we hope this may one day lead to a cure.”













