In a significant advancement for glioblastoma treatment, researchers at The University of Texas MD Anderson Cancer Center have discovered that natural killer (NK) cells engineered to express interleukin-21 (IL-21) show powerful and sustained antitumor activity against glioblastoma stem cell-like cells (GSCs).
Reporting in Cancer Cell, the scientists present the first evidence that IL-21 engineered NK cells could be an effective therapeutic approach for this aggressive brain cancer.
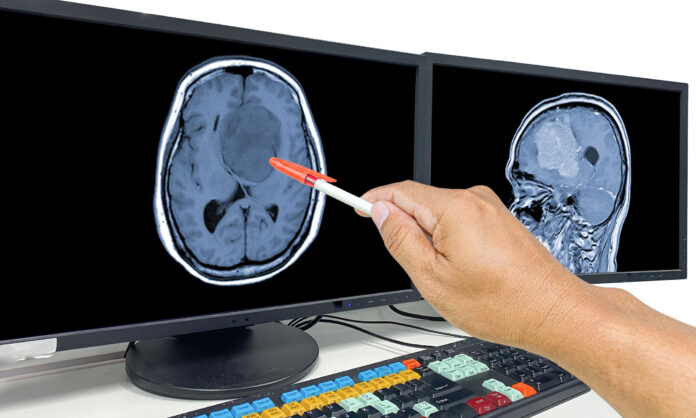
Glioblastoma is a highly aggressive brain cancer with limited treatment options, including surgery, radiation, and chemotherapy, which offer only modest survival benefits. The median survival time for glioblastoma patients is just 18 to 21 months, with a five-year survival rate of only 6.9%.
“Our research uncovered a previously unknown mechanism that plays an important role in NK cell memory against glioblastoma, highlighting the potential of NK cells engineered to express IL-21 in treating this disease,” said Katy Rezvani, MD, PhD, professor of Stem Cell Transplantation & Cellular Therapy at MD Anderson. “The ability of these IL-21 engineered natural killer cells to recognize and kill glioblastoma stem cell-like cells offers a highly promising therapeutic approach.”
NK cells are a type of innate immune cell with a natural ability to recognize and eliminate cancer cells, including GSCs. In this study, researchers engineered NK cells to express either IL-21 or IL-15, another cytokine known to enhance NK cell activity. While both types of engineered NK cells displayed strong antitumor activity in vitro, the IL-21 NK cells showed superior metabolic fitness and sustained activity compared to the IL-15 NK cells.
Using in vivo models, the IL-21 NK cells demonstrated excellent tumor control with limited toxicity, a significant improvement over IL-15 NK cells, which exhibited high toxicity and reduced effectiveness over time due to exhaustion.
The research team also identified the CCAAT/Enhancer-Binding Protein (C/EBP), particularly the transcription factor CEBPD, as crucial in regulating the sustained anti-GSC activity of IL-21 NK cells. Deleting CEBPD reduced the potency of IL-21 NK cells, while overexpressing it enhanced their long-term cytotoxicity, metabolic fitness, and antitumor efficacy.
“These results suggest that IL-21, through C/EBP transcription factors, drives epigenetic reprogramming of NK cells, enhancing their antitumor efficacy against glioblastoma,” the authors concluded in their publication.
Given the promising preclinical results, researchers at MD Anderson are preparing to investigate the clinical application of IL-21 engineered NK cells in patients with glioblastoma, with clinical trials anticipated to begin later this year.













