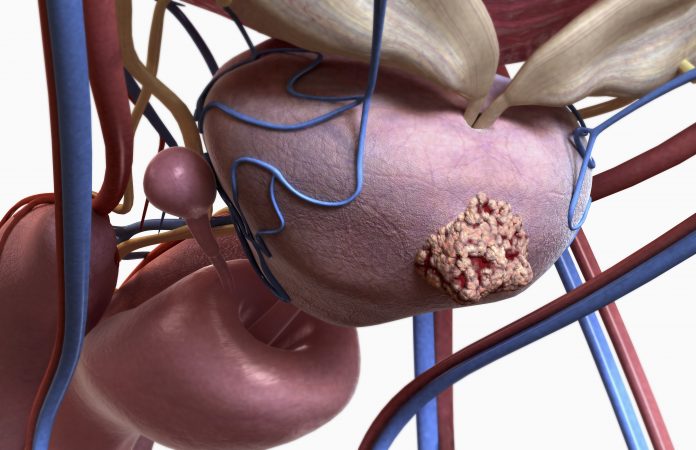
Researchers at Weill Cornell Medicine have uncovered a surprising role for the enzyme EZH2 in driving aggressive tumor growth in prostate cancers resistant to treatment. Published in Nature Communications, the study reveals that EZH2, regulated by the protein kinase PKCλ/ι, contributes to tumor progression by evading proteasomal degradation. These findings not only shed light on the mechanisms of resistance in castration-resistant prostate cancer (CRPC) but also highlight a potential therapeutic target for patients with limited treatment options.
The study is led by Maria Diaz-Meco, PhD, and Jorge Moscat, PhD, both Homer T. Hirst III Professors of Oncology in Pathology and members of the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine.
“Overcoming resistance to therapy is a major challenge in castration-resistant prostate cancer (CRPC), Lineage plasticity towards a neuroendocrine phenotype enables CRPC to adapt and survive targeted therapies,” the researchers wrote. “However, the molecular mechanisms of epigenetic reprogramming during this process are still poorly understood. Here we show that the protein kinase PKCλ/ι-mediated phosphorylation of enhancer of zeste homolog 2 (EZH2) regulates its proteasomal degradation and maintains EZH2 as part of the canonical polycomb repressive complex (PRC2).”
The scientists found that the absence of a protein called PKCλ/ι in prostate cancer cells enables EZH2 to drive aggressive growth, even with androgen receptor inhibitors present.
PKCλ/ι normally limits EZH2’s activity. However, in PKCλ/ι-deficient cells treated with androgen receptor inhibitors, an alternative form of EZH2 is produced that has a different function. Instead of repressing tumor-suppressor genes, this form of EZH2 drives rapid protein production and activates growth factors like TGF-β, fostering an environment around the tumor that promotes cancer progression despite androgen receptor inhibition.
“This study reveals a critical mechanism behind treatment resistance in prostate cancer, suggesting new therapeutic approaches,” explained Diaz-Meco. “By understanding EZH2’s role in this context, we may be able to re-sensitize tumors to androgen receptor inhibitors or make the cancer newly vulnerable to targeted treatments, such as immunotherapies.”
In preclinical studies, the team targeted EZH2’s alternative activities to assess potential treatment solutions. They observed that inhibiting either protein synthesis or the TGF-β pathway effectively reversed resistance in PKCλ/ι-deficient cancer cells. Blocking EZH2’s alternative function restored sensitivity to androgen receptor therapies like enzalutamide. Furthermore, since TGF-β is associated with immune suppression in tumors, inhibiting this pathway could enhance immunotherapy effectiveness, a treatment with limited success against prostate cancer alone.
The scientists noted that the absence of PKCλ/ι creates a unique vulnerability in cancer cells, suggesting that combining EZH2 inhibitors with AR-targeted therapies could significantly inhibit tumor growth. However, they caution that the inhibition of EZH2 in tumors with high levels of PKCλ/ι can sometimes counteract therapeutic effects, underscoring the need for precisely tailored treatments for patients with reduced PKCλ/ι levels. Given the complexity of the EZH2 pathway, achieving a careful balance is essential to avoid reversing treatment benefits.
The new study lays the groundwork for clinical trials combining androgen receptor inhibitors with EZH2 or TGF-β inhibitors for patients with therapy-resistant prostate cancer characterized by PKCλ/ι deficiency.













