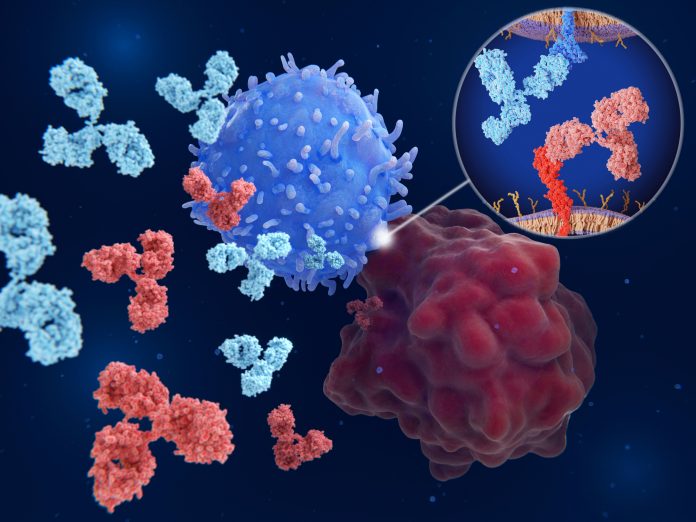
Immunotherapy, particularly with checkpoint inhibitors like the PD-1 inhibitor nivolumab and CTLA-4 inhibitor ipilimumab, has transformed melanoma treatment by leveraging the body’s immune system to target and destroy cancer cells. However, despite its effectiveness, this treatment can lead to severe grade 3–5 immune-related adverse events (irAEs), affecting over a third of patients and often forcing discontinuation of therapy. A recent study published in Clinical Cancer Research offers new insights into predicting these severe side effects, focusing on the role of spleen tyrosine kinases (SYK) in the immune response.
The irAEs related to immunotherapy can manifest as skin rashes, diarrhea, hyperthyroidism, liver toxicity, colitis, and autoimmune conditions like rheumatoid arthritis. The ability to predict which patients are at higher risk for these severe side effects would be a critical advancement, enabling oncologists to personalize treatment plans and potentially avoid life-threatening complications.
The study led by researchers at NYU Langone Health and the Perlmutter Cancer Center focused on the SYK pathway, a key signaling pathway involved in immune cell activation and response. The SYK pathway has been previously implicated in autoimmune diseases such as lupus, rheumatoid arthritis, and colitis, where the immune system mistakenly attacks healthy tissues.
“Unlike metastatic disease, where irAEs are a clinical trade-off for treatment that improves survival, the toxicity burden from immune checkpoint inhibition in adjuvant melanoma treatments is a substantial clinical problem urging for irAE-predictive biomarkers,” the authors write, emphasizing the purpose behind the study.
In their study, the researchers analyzed immune system cell samples from 212 melanoma patients enrolled in the CheckMate-915 trial, a multicenter clinical study designed to evaluate the effectiveness of combined immunotherapy with nivolumab and ipilimumab. The samples were collected before the start of treatment, allowing the researchers to assess whether certain gene activity patterns could predict the development of severe irAEs.
The analysis revealed a significant association between the activity of genes involved in the SYK pathway and the risk of developing severe irAEs. Specifically, the researchers identified a set of 24 genes that were differentially expressed in patients who later experienced severe side effects. Further statistical analysis narrowed down this gene set to five key genes—CD22, PAG1, CD33, HNRNPU, and FCGR2C—whose activity, along with patient age and melanoma stage, served as strong predictors of irAEs.
The researchers found that the SYK-related gene signature predicted approximately 60% of the combination-treated patients that experienced grade 3 to 5, or severe, irAEs. “This gene signature could serve as a baseline biomarker of severe grade 3–5 irAE risk, which is especially important in adjuvant therapy,” the authors write. This predictive model was found to be independent of the treatment’s effectiveness in preventing melanoma recurrence, indicating that the heightened activity of the SYK pathway is specifically related to the side effects rather than the therapeutic outcomes.
“Our results lay the foundation to create a pre-treatment blood-based biomarker for immunotherapy adverse events,” says co-lead investigator Kelsey Monson, PhD, emphasizing a potential breakthrough for identifying high-risk patients before starting immunotherapy. Such a test would enable oncologists to tailor treatment plans, possibly by opting for less aggressive immunotherapy regimens or implementing closer monitoring to catch and manage side effects early.
By incorporating predictive biomarkers like the SYK gene signature into treatment planning, oncologists could significantly reduce the risk of severe side effects, improving both patient outcomes and their quality of life.
The implications of this research extend beyond melanoma. The SYK pathway has been linked to various autoimmune conditions, and the study’s findings suggest that this pathway could serve as a biomarker for predicting side effects in other cancers treated with immunotherapy. The team plans to explore whether the SYK pathway’s activity can predict side effects in patients treated with ipilimumab alone or with other combination therapies.
Future research will also focus on understanding the mechanisms by which SYK pathway activation leads to severe irAEs. This knowledge could inform the design of new immunotherapies that retain their cancer-fighting capabilities while minimizing harmful side effects. Additionally, insights from this research could potentially be applied to developing treatments for autoimmune diseases, where the SYK pathway plays a critical role in disease progression.













