Certain biomarkers may predict likelihood of checkpoint inhibitor drugs “backfiring” during melanoma treatment. Duke Cancer Institute researchers have identified a pathway that may explain why this serious side effect occurs in a subset of patients.
Using a mouse model of melanoma, the team determined that an NLRP3 inflammasome (HSP70-TLR4) drives premetastatic cancer spread in the lungs, which is further enhanced by PD-1 blockade. These findings were mirrored by what the authors observed in melanoma patients. In the mouse model, genetic ablation or pharmacological inhibition of this signaling axis suppressed metastasis, suggesting this study points to a possible new clinical target.
The study appeared online Nov. 23 in Science Translational Medicine.
It’s estimated that up to 30% of cancer patients develop hyper-progression (HP) while on checkpoint inhibitors. These patients have a median overall survival of 4.6 months compared to 7.6 months in patients who don’t have this complication, which occurs in multiple tumor types, including melanoma, and cancers of the head and neck, lung, and breast.
“There is a continuum between resistance to immunotherapy and the development of a hyper-progressive state,” said Brent Hanks, MD, PhD, associate professor in the Department of Medicine at Duke University School of Medicine and senior author of the study.
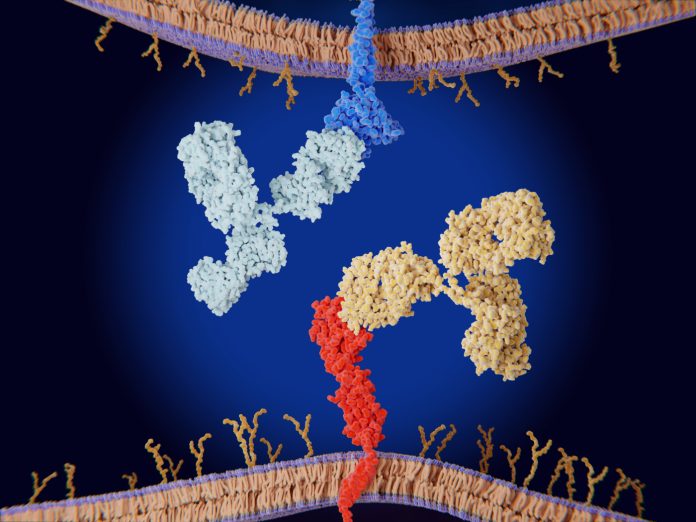
Checkpoint inhibitors have become one of the most successful drug classes of all time. Since the first such drug was approved in 2011, annual sales in this class have grown to $25 billion. These drugs include the PD1/PDL1 inhibitors Keytruda (Merck’s pembrolizumab) and Opdivo (Bristol Myers Squibb’s nivolumab).
“While hyper-progression occurs in a small percentage of cancer patients receiving checkpoint inhibitors, identifying the likelihood of this phenomenon has the potential to alter the clinical approach and avoid this complication,” Hanks said.
The tumor-intrinsic NOD-, LRR- and pyrin domain-containing protein-3 (NLRP3) inflammasome–heat shock protein 70 (HSP70) signaling axis typically recognizes foreign invaders. These researchers found that in tumors the NLRP3 inflammasome can activated T-cell responses and trigger a cascade of events causing resistance to the checkpoint inhibitors. Specifically, the tumor NLRP3-HSP70 axis also drives the accumulation of polymorphonuclear myeloid-derived suppressor cells (PMN-MDSCs) into distant lung tissues, which is a process dependent on lung epithelial cell Toll-like receptor 4 (TLR4) signaling. The inflammasome process can even help cancers spread.
The researchers followed up their mouse work by looking to identify which patients were at risk for developing hyper-progression prior to initiating checkpoint inhibitor immunotherapy.
Using tumor tissue samples from stage IV melanoma patients at Duke, they found that high baseline concentrations of the molecules involved in the inflammasome process were associated with the development of disease hyper-progression and inferior survival.
In addition, genetic and pharmacologic inhibition of NLRP3 and HSP70 blocked PMN-MDSC accumulation in the lung in response to anti–PD-1 therapy and suppressed metastatic progression in preclinical models of melanoma and breast cancer.
“We will be testing these biomarkers for their ability to predict both disease resistance and disease hyper-progression in response to checkpoint inhibitor immunotherapy in a larger cohort of melanoma patients,” he added.













