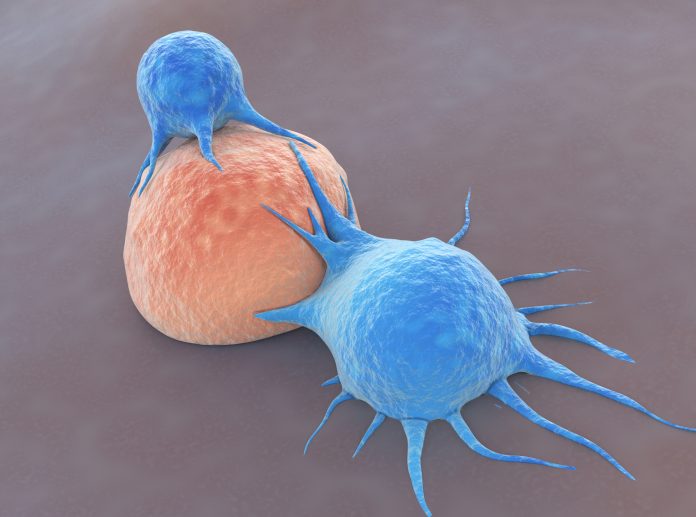
New research shows that using a chemical blocker stops CD8+ T cells from migrating out of skin cancer cells. Together with immunotherapy, the combination stopped melanoma tumor growth in half of treated mice, representing a potential new approach for boosting the efficacy of immunotherapy.
In a paper in Nature Immunology, researchers from NYU showed that the treatment, prevented the escape of CD8+ T cells within melanoma tumors, effectively doubling the number available to fight the cancer. Antigen-specific CD8+ T cell accumulation in tumors is a prerequisite for effective immunotherapy.
“We have known that T-cells migrate out of tissues,” said senior author, Amanda Lund, PhD, associate professor at NYU Grossman School of Medicine and Perlmutter Cancer Center. “But in the context of cancer, we haven’t understood the trafficking dynamics and how they impact the immune responses necessary for cancer therapy.” In this paper, her team revealed some of the important signals that draw T-cells out of tumors.
First, Lund’s team showed that CD8+ T cells escape melanoma tumors when they gather near the tumor periphery as well as nearby lymphatic vessels. Further experiments showed that signaling molecules found in the tumor microenvironment, specifically the chemokine CXCL12 and its related receptor protein CXCR4, attract and move T cells toward lymphatic vessels.
“When CXCL12 is made by inflamed, tumor-associated lymphatic vessels—which are the exit routes for T cells—it significantly alters where the T cells are, how they’re retained, and how they’re able to control the tumor,” added Lund. CXCL12 is not highly expressed in lymphatic tissue normally but is found in high levels within tumors. “So there’s something about the tumor that’s telling these vessels to make more and different kinds of chemokines that we think is important for pulling cells out of tissue.”
When researchers used a chemical blocker for either CXCL12 or CXCR4, T cells could not emigrate from the tumor and instead stayed in its center. The number of T cells in mice tumors doubled and half of them stopped growing.
“You can have a super T cell, but if it can’t get into the tumor and stay in the tumor, it doesn’t really matter,” said Lund. “What this paper shows is that it’s a dynamic process; it’s not just about getting something in, but it’s about whether or not it stays.”
Among the study’s other results was that T cell leakage depended on their potency, or how strongly they could bind to target proteins on tumor cells. The longer the most potent T cells spent inside tumors, the more likely they were to encounter their target cancer cells and the more likely these T cells were to remain inside the tumor. Increasing the initial time these T cells spend inside the tumor, the researchers say, may help improve therapy.
“Understanding the signals around what pulls out these T cells—and how to block them—will hopefully lead to better ways to improve their retention and therefore improve immunotherapy response,” said Lund. “There may be several ways to achieve it, but this paper shows that blocking the exit signals, either CXCR4 and/or CXCL12, shifts the balance in favor of keeping T cells inside of tumors long enough for immunotherapy to work.”
The team evaluated several blocking approaches: removing the CXCR4 receptor from T cells, removing the CXCL12 chemokine from lymphatic vessels, or using the small molecule inhibitor AMD3100. “In all three cases, we could improve T-cell mediated tumor control,” Lund noted.
Future research will look further into T cell blocking strategies to increase the “dwell time” of T cells inside tumors. Said Lund: “Once you’re able to drive potent immune responses within the tumor, if you can help the T cells stay in that space longer, we think it would boost response.”













