A multicenter study led by researchers at Sylvester Comprehensive Cancer Center at the University of Miami Miller School of Medicine has shown that interactions between tumor genes and microenvironment influence multiple myeloma treatment response in patients newly diagnosed undergoing combination treatments, including targeted immunotherapy. The study, published in in Nature Cancer, provides new insights crucial for understanding treatment responses and improving outcomes for multiple myeloma patients.
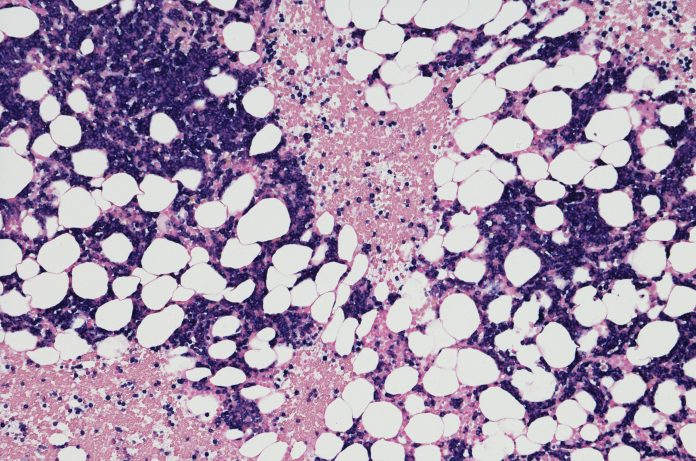
Over the last two decades, the development of new drugs has significantly enhanced survival rates for multiple myeloma, a cancer that affects plasma cells in the bone marrow. While, immunotherapies targeting the CD38 molecule on myeloma cells have shown efficacy, a substantial portion of newly diagnosed patients—between 30% and 50%—experience inadequate responses or premature progression.
“Since the introduction of advanced, targeted immunotherapy regimens, there has been a pressing need to better understand the tumor genomic and immune interactions that drive resistance to combination treatment approaches,” says senior co-author C. Ola Landgren, MD, hematologist/oncologist, chief of the Division of Myeloma and director of the Myeloma Institute at Sylvester. “This study adds significant information that will result in better clinical trials and more effective therapies for patients with high-risk disease.”
For this study, the researchers collected bone marrow samples from 49 patients treated with a combination therapy, including the CD38-targeting monoclonal antibody daratumumab. Employing whole-genome sequencing, they explored chromosomal changes in tumor cells that might increase the risk of treatment resistance. Additionally, single-cell RNA sequencing was used to analyze the tumor microenvironment, offering a detailed examination of the interplay between genomic features and immune microenvironment changes.
The findings revealed a complex interplay between tumor genomic features and immune microenvironment changes, influencing stronger treatment responses and prolonged progression-free survival. Importantly, the study identified instances where historically significant genomic prognostic factors lost predictive power with the introduction of immunotherapy. Conversely, new genomic drivers and microenvironmental features emerged as significant predictors of outcomes.
“We found that stronger treatment responses and prolonged progression-free survival were driven by a complex interplay between tumor genomic features and immune microenvironment changes,” notes Francesco Maura, MD, a co-first author of the paper and head of a laboratory at Sylvester that conducts myeloma computational and translational research. “Interestingly, we found that with the introduction of immunotherapy, some historically important genomic prognostic factors lost some of their power to predict outcome and a number of genomic drivers and microenvironmental features emerged as being of importance.”
The significance of these findings lies in their potential to guide the development of more effective therapeutic strategies. By understanding the dynamic relationship between tumor cells and the immune microenvironment, clinicians may be better equipped to tailor treatments for individual patients, addressing resistance mechanisms and improving overall outcomes for those diagnosed with multiple myeloma. This research contributes to the ongoing efforts to advance precision medicine in cancer treatment, bringing us closer to more targeted and personalized approaches for patients facing this challenging disease.













