Researchers at the Georgia Institute of Technology have developed lab-grown models of the human immune system that can be used to understand why some cancer patients are more susceptible to frequent infections even years after completing cancer treatment.
Known as human immune organoids, these miniature models of the human immune system address two key challenges for researchers and patients. First, when it comes to immunity, infection, and vaccine responses– especially in cancer treatment—there is a very low translation rate from preclinical research in animal models to effective clinical outcomes in humans. This means that the majority of therapies found to be working in animal models actually fail when tested in humans.
“While animal models are valuable for many types of research, they often fail to accurately mirror realistic human immune biology, disease mechanisms, and treatment responses,” commented Monica (Zhe) Zhong, PhD, the study’s first author, in a press release. “To address this, we designed a new model that faithfully replicates the unique complexity of human immune biology across molecular, cellular, tissue, and system levels.”
The second challenge addressed by these new human immune organoids is that many cancer patients, especially those treated with immunotherapies, often suffer from frequent infections due to reduced antibody production. These infections can occur even years after the cancer treatment is completed.

The paper was published in the journal Nature Materials. In the study, the researchers used their human immune organoids to test why some lymphoma survivors treated with CD20-targeted immunotherapies suffer from these lowered immune defenses. They found that the immune cells of lymphoma survivors don’t organize themselves in the same way as they would in a strong immune response, namely, in “zones.”
“[…] Understanding these long-term impacts on antibody responses could be key to improving both safety and quality of life for lymphoma survivors,” explained Jean Koff, MD, co-author of the paper and associate professor in the department of hematology and oncology at Emory University’s Winship Cancer Institute, in a press release.
“This technology provides deeper biological insights and an innovative way to monitor for recovery of immunological defects over time. It could help clinicians better identify patients who would benefit from specific interventions that reduce infection risk.”
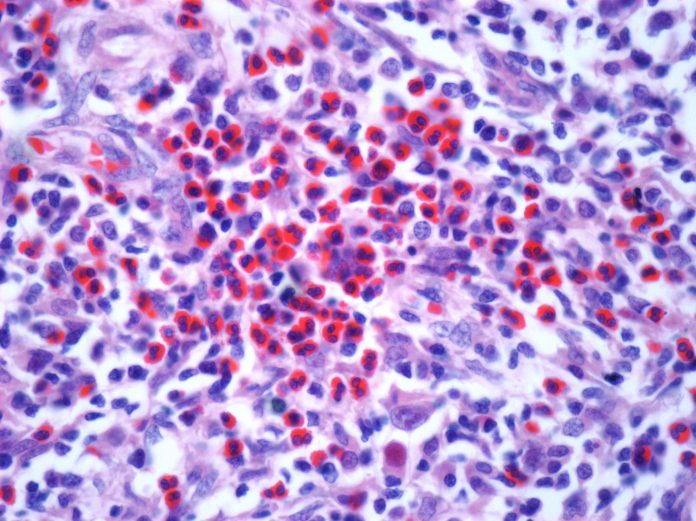
To recreate the human immune system in miniature, the research team developed a gel-like microenvironment using synthetic hydrogels in which B cells taken from human blood and tonsils are able to mature, grow, and produce antibodies. Within these human immune organoids, immune cells from healthy donors and lymphoma patients can live and function for longer, allowing researchers to study different cellular processes, such as antibody formation, or responses to novel therapies.
Ankur Singh, PhD, the Carl Ring Family Professor in the George W. Woodruff School of Mechanical Engineering and Professor in the Wallace H. Coulter Department of Biomedical Engineering at Georgia Tech and Emory, said in a press statement:
“For the first time, we can recreate and sustain complex immunological processes in a synthetic gel, using blood, and effectively track B cell responses. […] At the end of the day, this work most immediately affects cancer patients and survivors, who often struggle with weakened immune responses and may not respond well to standard treatments like vaccines. This breakthrough could lead to new ways of boosting immune defenses, ultimately helping vulnerable patients stay healthier and recover more fully.”
The research team plans to further explore the potential of its human immune organoids, for example, by working on cell therapies and modeling the aged immune system to observe age-related diseases. Other researchers are developing organoids to develop personalized cancer therapies, for more precise treatment selection, or to better understand certain cancers.













