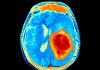
Research led by Cold Spring Harbor Laboratory shows that chronic stress increases metastasis in mouse models of breast cancer through a mechanism whereby stress hormones trigger neutrophils to form spider-web-like structures that create a metastasis-friendly environment.
“These stress-induced NETS [neutrophil extracellular traps] play a role in promoting the metastasis of breast cancer by creating a favorable environment in the lungs that helps the breast cancer cells that reach the lung grow more easily,” said senior author Mikala Egeblad (now a Bloomberg distinguished professor with Johns Hopkins University).
She told Inside Precision Medicine: “This new finding helps us better understand how stress can impact the spread of cancer and may provide new opportunities for treating and preventing metastasis.”
Egeblad’s lab has long-studied how the communication between tumors and the immune system affects tumor growth and metastasis in mice. During previous work they happened to find that a change in housing conditions caused some mice to experience stress, which resulted in much faster tumor growth.
“This discovery sparked our curiosity to understand whether and how chronic stress exposure can impact metastasis,” remarked first author Xueyan He, who was a postdoc at Cold Spring Harbor Laboratory at the time of the study and is now assistant professor of cell biology & physiology at the Washington University School of Medicine.
She added: “While epidemiological studies show an association between stress and an increased risk of cancer metastasis and shorter survival, it remains very challenging to study how stress specifically affects the body and the cancer.”
“This is particularly important for cancer patients who undoubtedly experience stress due to e.g., concerns about their diagnosis, worries about recurrence, and potential long duration of their treatments, therefore, we decided to use mouse models to simulate chronic stress and study the spread of breast cancer.”
The researchers report in Cancer Cell that chronic stress approximately doubled the size of mammary tumors in mice transplanted with breast cancer cells and increased the rate of metastasis between two- and four-fold, compared with mice not exposed to stress.
They then showed that chronic stress significantly alters the lung microenvironment, with fibronectin accumulation, reduced T cell infiltration, and increased neutrophil infiltration. Yet, in neutrophil-depleted mice, stress exposure no longer increased metastasis.
“Together, these data show that chronic stress induces a pro-metastatic lung microenvironment and that neutrophils play a key role in orchestrating stress-induced metastasis,” the study authors write.
Further analysis revealed gene expression changes in neutrophils isolated from the lungs of stressed mice that were primarily caused by the presence of glucocorticoids, hormones involved in the stress response.
In addition, shifts from the normal circadian rhythm of neutrophils because of increased stress led to increased NET formation via glucocorticoid release.
To confirm that stress triggers NET formation, leading to increased metastasis, He and team performed three more tests. First, they removed neutrophils from the mice using antibodies. Next, they injected a NET-destroying drug into the animals. Lastly, they used mice whose neutrophils couldn’t respond to glucocorticoids. Each test achieved similar results—the stressed mice were no longer developed more metastases than those not exposed to stress.
Unexpectedly, the investigators also found that chronic stress caused NET formation to modify lung tissue even in mice without cancer. “It’s almost preparing your tissue for getting cancer,” said Egeblad.
The researchers point out that their study could have implications for the use of synthetic glucocorticoids, such as dexamethasone, which are widely used to overcome the side effects of chemotherapy and to treat symptoms of advanced cancer.
They showed that dexamethasone can cause NET formation and make the lung environment favorable for the metastatic cancer cells, suggesting that synthetic glucocorticoids might not always be beneficial in the long term.
However, He stressed that “studies are needed to fully address whether synthetic glucocorticoids have potential[ly] overlooked longer term risk. Importantly, we did not find any strong evidence that patients should worry about prescribed synthetic glucocorticoids— likely the positive effects of glucocorticoids balance out any potential long-term harm.”
A take home message from the study is that “reducing stress should be a very beneficial part of cancer treatment and prevention,” said Egeblad. “Since reducing stress can be difficult for cancer patients, we also speculate that drugs preventing NET formation can be developed and used as new treatments to slow or stop cancer’s spread, offering much-needed relief.”
The researchers will continue to investigate how stress influences cancer progression and plan to explore the impact of various stress reduction techniques, such as behavioral interventions or pharmaceutical interventions.
“Our understanding of the complex relationship between stress, glucocorticoids, neutrophils and other immune cells and cancer progression is still very nascent. But we hope further studies will pave the way for interventions and treatments that can improve patient survival,” said Egeblad.