People with mantle cell lymphoma (MCL) who go into remission after initial therapy may not need an autologous stem cell transplant, a procedure that tends to be recommended for people with this type of cancer.
Results from a study, presented at the 66th American Society of Hematology (ASH) Annual Meeting in San Diego, showed three-year overall survival rates for people in remission with MCL who were treated with immunotherapy (rituximab) alone versus immunotherapy and a stem cell transplant were very similar.
“In this interim analysis, MCL patients in first complete remission with undetectable minimal residual disease did not benefit from consolidative autologous stem cell transplant,” said lead researcher Timothy Fenske, MD, a professor of medicine at the Medical College of Wisconsin, who presented the results at the conference.
“Patients who remain minimal residual disease-positive after induction may benefit from autologous stem cell transplant. Longer follow-up will be important to confirm these findings.”
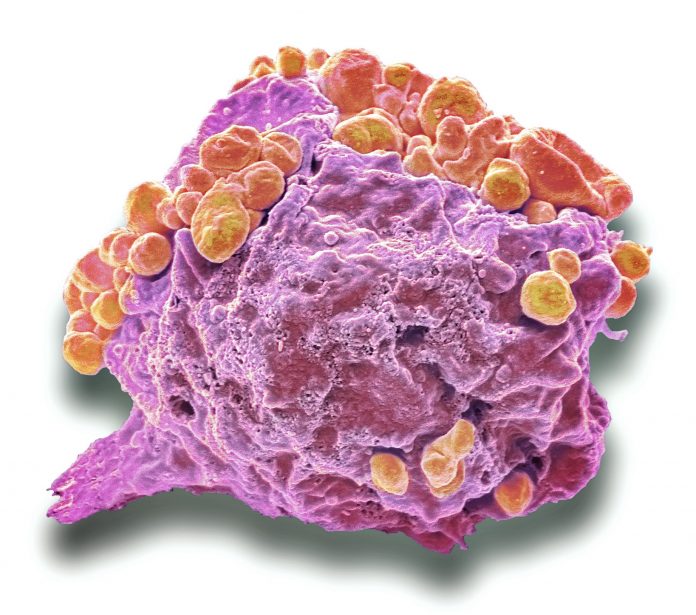
MCL cases account for around six percent of non-Hodgkin lymphomas. This cancer is named for the mantle zone of the lymph nodes where it develops. Prognosis for MCL used to be a lot worse, but treatments such as the monoclonal antibody rituximab have improved outcomes and a first remission after treatment can now last as long as 10 years.
One treatment option often suggested for people with MCL is an autologous stem cell transplant, but this is a serious procedure that involves blood stem cell extraction from the patient, high dose chemotherapy, and then reinfusion of their own stem cells. While it is often effective, it can be very tough on patients.
In this study, 650 people, aged 18–70 years, with MCL in first remission were enrolled— 257 to arm A (stem cell transplant plus rituximab for three years) and 259 to arm B (rituximab for three years). An additional 134 people recruited to the study (groups C and D combined) were positive for minimal residual disease or had uncertain results and were all given an autologous stem cell transplant plus maintenance rituximab treatment for three years.
For those with no detectable disease, three-year overall survival rates for people who were treated with chemotherapy (rituximab) alone versus chemotherapy plus a stem cell transplant were 82.7% vs 82.1%. This led to the study being stopped after the interim analysis as there was no notable difference between treatment groups.
“EA4151 is the first randomized trial to study autologous stem cell transplant for MCL patients with undetectable minimal residual disease in first remission, within an era of highly effective induction and maintenance regimens. The benefit of ASCT in this current era has been debated heavily, because the data suggesting benefit of ASCT all came from the context of older trials and treatments,” noted Fenske, adding that “longer follow-up will be important to confirm these findings.”













