Researchers at Weill Cornell Medicine have identified a new biomarker that could help predict which patients with hepatocellular carcinoma (HCC), the most common form of liver cancer, are likely to benefit from immunotherapy. The findings, published today in Molecular Cell, detail the role of two proteins, p62 and NBR1, and their opposing functions in regulating interferon response in hepatic stellate cells, an important component in the liver’s immune response against tumors.
The study showed that elevated levels of NBR1 in hepatic stellate cells could indicate a poor response to immunotherapy. Conversely, high levels of p62 may offer protective effects against cancer by enhancing the immune response. Importantly, the investigators demonstrated that lowering NBR1 in animal models of the disease shrank tumors, making it an important new therapeutic target that could enhance immunotherapy response.
“P62 and NBR1 are yin and yang,” said the study’s co-principal investigator Jorge Moscat, MD, PhD, a professor of oncology in pathology at Weill Cornell Medicine. “In contrast to NBR1, if p62 is high in hepatic stellate cells, a patient is protected from cancer, but if it is low, the immune system is knocked down. If NBR1 is high, the immune system is impaired, but if NBR1 is low, the immune response increases.”
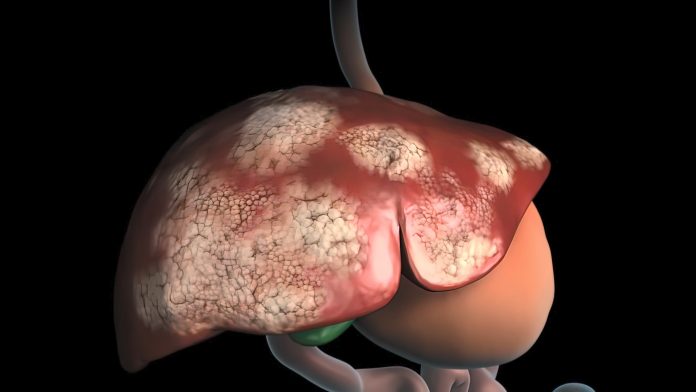
Hepatocellular carcinoma patients typically have a poor prognosis and few treatment options with available options for treatment typically only extending life by a few months. While immunotherapy has provided a new alternative that can extend a patient’s life by as much as two years, only 15–30% of patients respond show any response.
An additional complication for treating physicians is the lack of predictive biomarkers to indicate which patients will respond to immunotherapy and which ones won’t.
“We need biomarkers to identify which patients will respond and who will achieve long-term survival,” said co-principal investigator Maria Diaz-Meco, MD, PhD, also a professor of oncology in pathology at Weill Cornell Medicine, who also noted the therapeutic potential of the team’s research: “The liver is an organ that is tremendously immune suppressed. Reactivating the immune system is a very attractive approach that is now bearing fruit.”
For their research, the Weill Cornell team sought to identify biomarkers and potential therapeutic targets by searching for what goes awry in the liver’s healing mechanisms that can eventually lead to cancer. They focused on the tumor-suppressing protein p62, the levels of which previous studies have shown is irreversibly depressed in hepatocellular carcinoma patients.
Their investigation showed that p62 helps promote immune response by activating the STING protein. This activation pushes the NBR1 protein out of the way, triggering an immune response that attacks the tumor. NBR1 was shown to breakdown STING and block immune response and when NBR1 was deleted from hepatic stellate cells in the mouse models of the disease, the immune response is “rescued” even when p62 levels remain low.

“If we don’t fully comprehend the molecular mechanisms regulating these processes, immunotherapy will not progress, and we won’t be able to understand why it works in some patients and not others,” Diaz-Meco concluded.













