Researchers at the University College London (UCL) and UCL Great Ormond Street Institute of Child Health have developed a novel immunotherapeutic platform technology that uses engineered T cells to attack bone cancer cells and activate other cancer-fighting immune cells to do the same.
The researchers aimed to overcome different challenges that current immunotherapies have in treating solid tumors. Immunotherapies that use genetically engineered cells to attack cancer cells work well in blood cancers, but they have yet to perform properly in solid tumors.
These types of immunotherapy, such as CAR-T cell therapy, also have to be designed using the cancer patient’s own T cells. The use of donor T cells would make these therapies more accessible and cheaper.
“We now know a lot more about different parts of the immune system than we did when immunotherapy was first developed,” Jonathan Fisher, PhD, senior author of the study, group leader at UCL Great Ormond Street Institute of Child Health, and a pediatric oncology consultant at UCL Hospital, told Inside Precision Medicine.
“We went back to the start and tried to use and choose bits of the immune system that we could put together to make a platform that was specifically designed for solid cancers. The cell type we are using can be taken from a donor and safely given to a patient, which means that you can do all the engineering at scale beforehand, so one donation might make enough for more patients.”
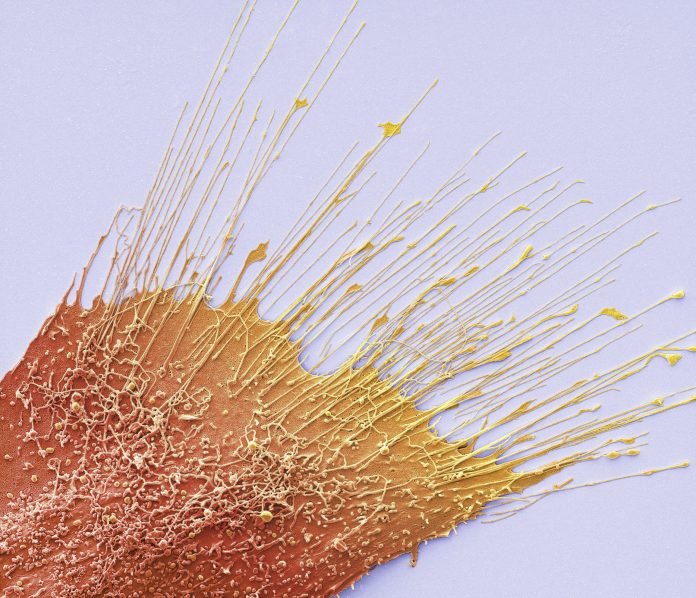
In their paper, published in the journal Science Translational Medicine, the researchers describe how they engineered a type of T cell known as gamma-delta T cell to secrete a synthetic antibody that can target bone cancer cells. The engineered T cells also release cytokines that make the cells more cytotoxic and activate other immune cells in the tumor microenvironment.
“We’re calling this new immunotherapeutic platform a multi-modal payload delivery system rather than a cellular therapy because the T cells secrete this payload into the vicinity of the tumor. The engineered cells kill the cancer and then bystanders get activated and help kill the cancer as well,” Fisher explained.

Moreover, the researchers were able to enhance the anti-cancer activity of their engineered T cells by adding zoledronic acid, a bone-strengthening drug that binds to the bone and is known to activate gamma-delta T cells in the blood.
“If you think about it in an arc, we would engineer the T cells in the lab and then give them to the patient,” Fisher said. “They’d go into the patient’s bloodstream where they would release the cytokine chemical and the antibody, and then we would give the patient the bone-binding drug, and quickly, all the sensitization ends up in the bones. This means that you can specifically target cancer that is in the bone.”
Primary bone cancer like osteosarcoma is rare. In the future, the researchers want to extend their research to secondary bone cancers, and as a next step, get funding to do a first-in-human study in patients with secondary bone cancers.
“One of the massive unmet needs is cancer that has spread from other parts of the body into the bones because it is very difficult to treat and there aren’t many treatments available for these patients. Whilst we’ve modeled the immunotherapeutic platform in osteosarcoma, the intention is to now take this to secondary bone cancers as well because thousands of patients could potentially benefit from that.”













