Researchers observed that cells that are present in cancerous brain cells but not in normal brain tissue—known as cancer-associated fibroblasts (CAFs)—secrete a protein that stimulates breast cancer cells in the brain to migrate and invade more widely. The excreted protein, fucosylated poliovirus receptor (PVF), was shown in mouse models to stimulate breast cancer migration and invasion.
The researchers from the Moffitt Cancer Center focused on CAFs, which are not cancer cells, but non-cancerous, non-immune stromal cells that surround the cancer. Through secretion of growth factors, CAFs are well-known to drive cancer cells to metastasis, including breast cancer cells, to different organs; however, their roles in brain metastasis are less defined. The team found that the secretion of PVR from the fibroblasts is triggered by its fucosylation, a type of protein modification in which the sugar L-fucose is added to proteins, impacting their behavior and functions. Their fidnings are published in Cell Reports.
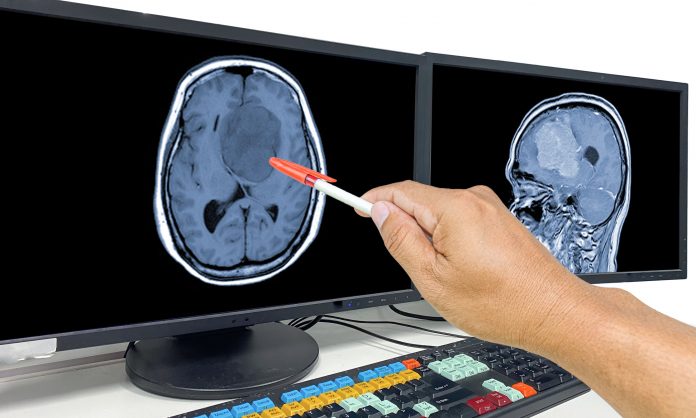
“Once the metastatic cells arrive in the brain, they have to burrow out of blood vessels and cross into the brain,” senior author Eric Lau, PhD, of the Department of Tumor Microenvironment & Metastasis at Moffitt. This research reveals its fibroblasts that secrete fucosylated PVR as a mechanism that helps the metastatic cells invade deeper into the brain.
“Fucosylation of PVR on this fibroblast makes the protein secrete out of the fibroblast cells, and then when they get in contact with the breast cancer cells, those breast cancer cells acquire the phenotype that is required to burrow out of the brain and spread more widely in the brain,” explains first author Emma Adhikari, PhD, formerly of the Lau lab, now establishing her own lab at Moffitt.
In their experiments, the team injected breast cancer cells alone or with fibroblasts that either do or do not secrete fucosylated PVR. “The difference was night and day,” adds Lau. Breast cancer cells alone proliferated at a local spot. The same was true for cancer cells attached to fibroblasts with non-fucosylated PVR. “But the cells in the presence of fibroblasts secreting fucosylated PVR, they burrowed deeper and more widely,” he says. Clinically, the result is multi-metastasis in the brain where the cells interfere with brain function and start the process of manifesting neurological symptoms with a poor prognosis.
The team hopes the discovery of the role of this secreted protein can serve as an earlier biomarker of brain metastasis. The protein is secreted into the blood vasculature and the cerebral spinal fluid circulation—two types of circulating fluid to the brain that secreted PVR can infiltrate. “So rather than a scan or any invasive procedure, maybe just taking a blood sample or taking a cerebral spinal fluid sample and testing for high levels of fucosylated PVR might help diagnostically,” says Lau. “If there are high levels, maybe that suggests that lesions are already there, that these cancer cells and fibroblasts are together, and this metastatic process has started.”
The Moffitt researchers also discovered many other signaling pathways that change in breast cancer cells as soon as they encounter PVR. “There is no good therapeutic for brain metastasis right now,” adds Lau. “But if we know that the breast cancer cells are hanging out with these fibroblasts and the fibroblasts are secreting PVR and it’s stimulating these signaling changes, maybe we target those signaling changes.”
The team plans to target some of these newly identified signaling changes with inhibitors of these pathways. “There is the potential that depending on where the cancer-associated fibroblasts arise and how they are moving with the cancer cells, there is potential that they might impact other metastatic cascade as well,” says Adhikari.











