Triple-negative breast cancer (TNBC), the most aggressive and difficult-to-treat form of breast cancer, may soon have a new treatment option. Researchers from the Brigham and Women’s Hospital, part of the Mass General Brigham healthcare system, have identified a promising therapeutic strategy that combines two types of drugs, setting the stage for potential clinical trials. The study, recently published in Nature, highlights how a combination of EZH2 and AKT inhibitors can selectively target and kill TNBC cells.
TNBC is known for its high recurrence rate and poor prognosis, as standard treatments like chemotherapy and immunotherapy often provide only short-term responses. To address this, the research team led by Karen Cichowski, PhD, from the division of genetics at the Brigham and Women’s Hospital, investigated a novel approach by combining EZH2 inhibitors, which target epigenetic changes, with AKT inhibitors, which target the PI3K pathway—a pathway altered in over 70% of TNBC cases.
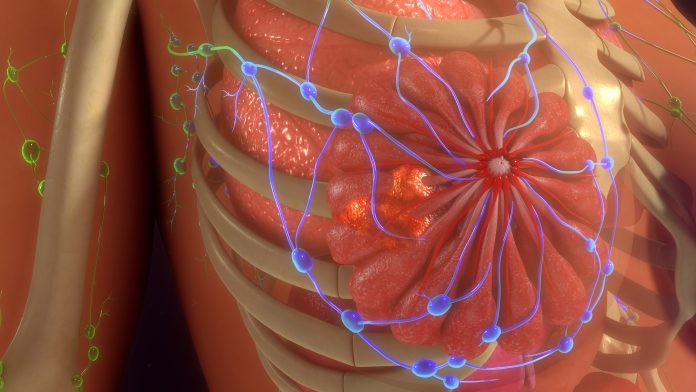
The team discovered that these two agents work together to induce a process called differentiation in TNBC cells, shifting them into a state that more closely resembles healthy, non-cancerous cells. Once differentiated, the tumor cells become vulnerable to cell death through a mechanism similar to mammary gland involution. Involution is a natural process that occurs when breast tissue returns to a non-lactating state after breastfeeding ends. By leveraging these natural signals, the combined therapy effectively eliminates TNBC cells in patient-derived samples used in the study.
“When combined, these therapeutic agents can hijack signals that occur naturally in the body to eliminate breast cells after lactation to kill these aggressive cancer cells,” said Dr. Cichowski. “Our results provide compelling support for the development of clinical trials to test whether combining these agents could benefit patients with TNBC.”
In their experiments, the researchers used machine learning to develop a predictive model that could forecast which patients would respond best to this combined treatment. This model, based on the interaction between EZH2 and AKT inhibitors, could be a valuable tool in selecting patients most likely to benefit from this therapy. By applying machine learning, they were able to identify key patterns in how TNBC cells responded to the drugs, providing a foundation for future clinical trials.
The study also revealed insights into how TNBC cells use epigenetic enzymes like EZH2 to protect themselves from conventional treatments. These enzymes help insulate the tumor cells, making them more resistant to therapies. By inhibiting EZH2, the researchers were able to disrupt this protective barrier, allowing the AKT inhibitors to drive the cancer cells into a more vulnerable, differentiated state. Once in this state, the cancer cells are susceptible to signals that trigger programmed cell death, making the therapy highly effective.
Based on these promising results the researchers believe that similar therapeutic combinations could be explored for other types of cancer with similar characteristics. The scientists hope to expand their studies to test the effectiveness of EZH2 and AKT inhibitors in additional tumor types and plan to move forward with clinical trials to evaluate the safety and efficacy of this combination treatment in TNBC patients.





![Comprehensive Genomic Profiling at Diagnosis Extends Survival in Patients with Advanced Cancer Harmonizing NGS standards is expected to provide a strong evidence base for decisions on coverage of clinical genomic testing and treatment for cancer. [iStock / zmeel]](https://www.insideprecisionmedicine.com/wp-content/uploads/2019/01/507-218x150.jpeg)







