Adaptimmune’s pivotal SPEARHEAD-1 trial has shown that the T cell receptor therapy afami-cel effectively targets metastatic synovial sarcoma and myxoid round cell liposarcoma, potentially opening the door for other solid tumors to be treated with T cell therapies.
“Synovial sarcoma is a rare cancer with historically limited treatment options and poor prognosis for advanced patients who fail first line treatment,” explained Dennis Williams, Adaptimmune’s senior vice president of late-stage development. “The five-year overall survival rate for advanced patients is just 20 percent, and this patient population has not had a new treatment option in more than a decade. There is a high unmet medical need.”
He told Inside Precision Medicine that afami-cel, short for afamitresgene autoleucel, demonstrated early potential “to transform the treatment landscape for people with synovial sarcoma,” with a response rate of 44 percent in a phase I trial among patients with late-stage, metastatic disease.
The current phase II, SPEARHEAD-1 trial, published in The Lancet, included 44 heavily pre-treated patients with metastatic or unresectable synovial sarcoma and eight patients with myxoid round cell liposarcoma, a distinct disease that shares clinical and biological features with synovial sarcoma including the expression of the MAGE-4 cancer antigen.
They were given a single dose of afami-cel after undergoing lymphodepletion with cyclophosphamide and fludarabine.
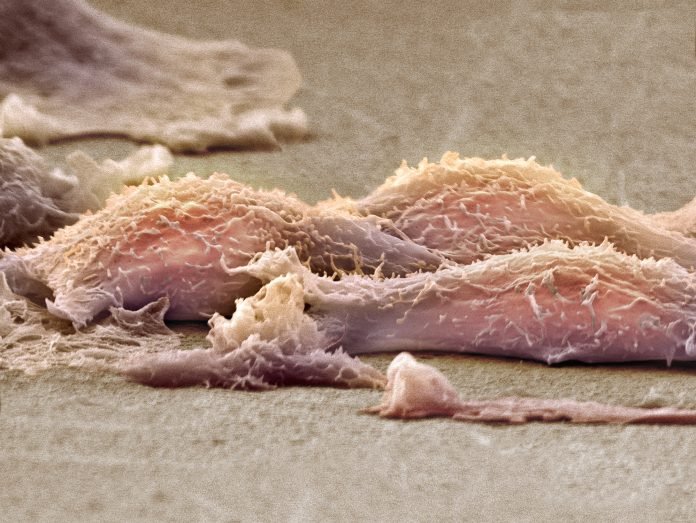
“Afami-cel is a therapy derived from a patient’s own immune system,” said senior study author Brian A. Van Tine, professor of medicine at Washington University. “When a synovial sarcoma [or myxoid round cell liposarcoma] patient is found to have both the expression of a tumor protein called MAGE-A4 and a specific immune system subtype called HLA02, we are able to modify a patient’s own T-cells to attack their cancer. As this treatment is derived from a patient’s own cells, it is a single treatment that allows a patient to treat themselves for a prolonged period of time.”
During a median follow-up period of 33 months, 39 percent of patients with synovial sarcoma had a treatment response, as did 25 percent of those with myxoid round cell liposarcoma, which represents a substantial improvement for this patient population where objective response rates with current second-line and beyond therapies range from 4–18 percent.
The median time to a confirmed response was 4.9 weeks, while the median response durations were 11.6 months in patients with synovial sarcoma and 4.2 months in those with myxoid round cell liposarcoma.
For patients with synovial sarcoma, median overall survival was not reached but the researchers estimated that 90 percent of those with a response would be alive at 12 months, and 70 percent would be alive at 24 months.
Hematologic toxicities were the most common adverse events, which the investigators say was expected and “largely due to lymphodepletion chemotherapy.” Specifically, 96 percent of patients experienced grade 3 or worse lymphopenia, 85 percent had grade 3 or worse neutropenia, and 81 percent grade 3 or worse leukopenia. Cytokine release syndrome, an adverse event of special interest that occurs after treatment with some types of immunotherapy, occurred in 71 percent of participants overall, but the majority of cases were grade 1 or 2 in severity.
“Afami-cel’s proof of principle study in synovial sarcoma will hopefully allow for the first FDA [the U.S. Food and Drug Administration] approval of an engineered T-cell therapy in a solid tumor,” Van Tine told Inside Precision Medicine. “Given that 1–3 percent of all solid tumor patients may express MAGE-A4 and have the HLA02 immune system subtype, this category of therapy may have broad applicability as a precision medicine.”
In January 2024, Adaptimmune announced that the FDA has accepted its Biologics License Application (BLA) for afami-cel for priority review. The application has a Prescription Drug User Fee Act target action date of August 4, 2024.
“If this BLA is granted, afami-cel provides a very high quality of life without the need for additional infusions as a patient’s treatment comes from their own cells that live in their body,” Van Tine remarked. “This is a huge advance in a therapy for a rare tumor that was in need of a paradigm shift in therapeutic approaches.”
Williams added that afami-cel is also currently being studied in children and young adults with malignant peripheral nerve sheath tumors, neuroblastoma, or osteosarcoma.
In addition, Adaptimmune is developing another next generation T-cell therapy, uza-cel (formerly ADP-A2M4CD8), for priority indications including ovarian cancer, head and neck, and bladder cancer.
“What differentiates this therapy from afami-cel is that these cells also express the CD8α co-receptor alongside the engineered T cell receptor that targets MAGE-A4,” said Williams. “Preclinical data indicated that co-expression of CD8α may broaden the immune response against solid tumors and increase anti-tumor activity.”













