Two studies published in The New England Journal of Medicine have shown that although the risk for secondary T-cell lymphoma is low after CAR T cell therapy, it is not nonexistent, and clinicians should be aware that patients may be susceptible to this outcome.
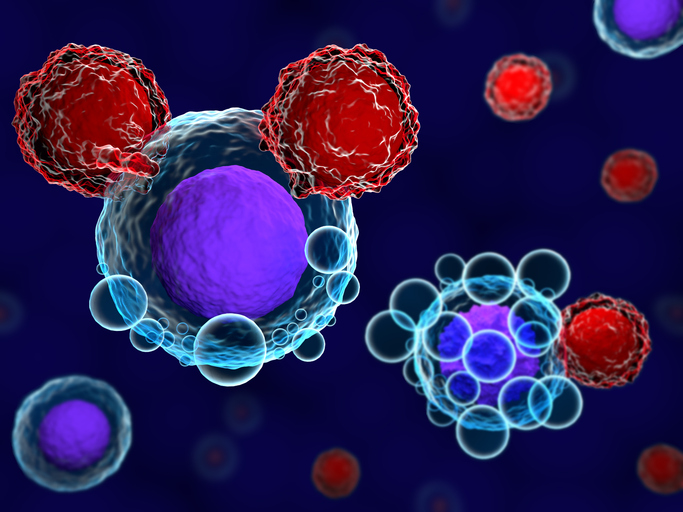
CAR T cell therapy is an effective treatment for hematologic cancers that uses a patient’s own genetically modified T cells. The cells are modified to express a chimeric antigen receptor (CAR) gene that is engineered to code for a transmembrane protein with extracellular antigen recognition and intracellular T cell–activating domains that enable CAR T cells to recognize and attack cancer cells that express its target antigen.
The therapy can be associated with serious immune-related side effects and in November 2023, the U.S. Food and Drug Administration (FDA) issued a warning about an increased risk for secondary cancers. The warning was driven by increasing concern following reports of patients diagnosed with T cell cancers unrelated to the cancer for which they had been treated.
To investigate the real-world risk, Mark Hamilton and colleagues from the Stanford Cancer Institute reviewed data for 724 patients who had received T cell therapies at their center since 2016.
They identified 25 patients who developed second tumors, excluding nonmelanoma skin cancers. Of these, 14 cases involved second hematologic tumors, including 13 cases associated with myelodysplastic syndrome or acute myeloid leukemia and one T cell lymphoma. This corresponded to a three-year cumulative incidence for hematologic second tumors of 6.5%, which the researchers say “reflects the rarity of an incident second tumor after CAR T-cell therapy as previously reported.”
Further analysis of the secondary T cell lymphoma case, which proved fatal, found that it was likely due to the immunosuppression caused by CAR T cell therapy, rather than the CAR T cells specifically.
“We wanted to understand this one rare case, so we analyzed all the patients treated with CAR T cell therapy at Stanford with wide breadth and studied this single case extraordinary depth,” said Ash Alizadeh, senior author and professor of medicine. “We compared protein levels, RNA sequences and DNA from single cells across multiple tissues and time points to determine that the therapy didn’t introduce the lymphoma into this patient; instead it was already brewing in their body at very low levels.”
In the second paper, Metin Ozdemirli, from Georgetown University Hospital, and co-authors report a case study of a patient who developed progressively worsening non-bloody diarrhea four months after receiving CAR T therapy for multiple myeloma. The symptoms initially resembled an autoimmune disease, with duodenal ulcers detected by endoscopy, but further testing revealed indolent T cell lymphoma of the gastrointestinal tract.
Unlike the case described by Hamilton et al., Ozdemirli and team found that the lymphoma likely originated from the CAR T cells.
It is unclear how the CAR T cells became a lymphoma but it could be that the cells had lymphoma-causing mutations when they were originally collected from the patient and CAR T treatment caused activation and expansion of those cells. Alternatively, the mutations might have occurred when the CAR T cells were prepared outside the patient or the CAR T cells may have acquired the mutations after they were given back to the patient, or any combination of these circumstances.
At present, no steps are taken to mitigate the risk for secondary T cell cancers after CAR T cell therapy.
“As of today, we do not have enough definitive evidence that CAR T therapy increases the risk of secondary T cell lymphomas and more importantly the mechanisms of how it does this are unknown,” Ozdemirli told Inside Precision Medicine. “Thus, suggesting any preventive measures will be too premature. However, based on our case, previously described cases and FDA reports of other cases, preventive measures such as screening for minor T cell clones before CAR T therapy and improving CAR vectors may be considered.”
Alizadeh believes the question of how to improve surveillance and awareness of T cell lymphoma after CAR T cell therapy “remains a largely open.”
He said: “Given the impact of CAR T cells as potentially life-saving therapies for control of lethal malignancies, it remains to be seen whether the small risk of secondary malignancies including T cell lymphomas might ever be cause for withholding curative therapies in patients with otherwise unmet needs. Nevertheless, given that several reports have now found the infused CAR T cells to directly contribute to secondary T cell lymphomas as confirmed by the presence of the engineered viral transgenic vectors within the T cell tumors, it would seem prudent to better study this process through active surveillance and vigilance.”
Alizadeh noted that the FDA currently requires a minimum 15 years of follow-up for patients given human gene therapy products and suggests that “noninvasive monitoring and surveillance of engineered vectors during this period could help intercept emerging T cell lymphomas towards their more efficient early eradication at the smallest tumor burden.”
Ozdemirli agrees that better surveillance and awareness of T-cell lymphoma is needed among patients given CAR T cell therapy. He said: “Based on our study, clinicians and pathologists need to be aware of possibility of indolent (low grade) CAR T cell lymphoproliferative disorders mimicking autoimmune or reactive conditions. In these cases, clonality of T cells and presence of CAR vector need to be investigated.”













