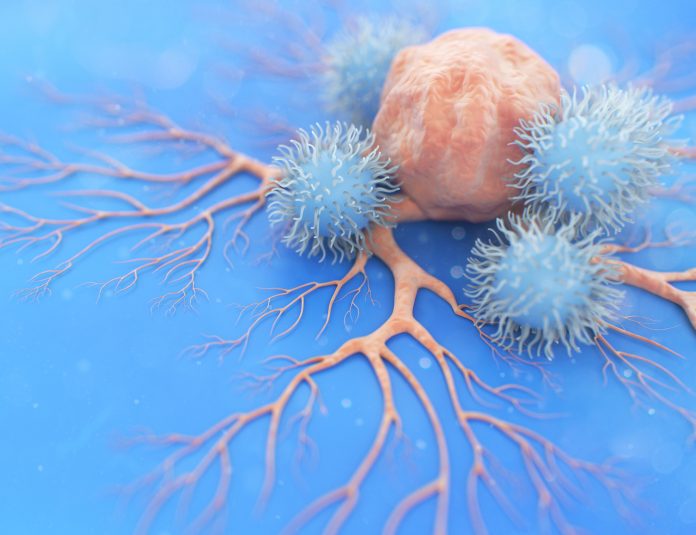
A new study uncovers why natural killer (NK) cells stop actively attacking tumor cells once they infiltrate cancers and possibly offers a way to boost their activity. The researchers, from the University of Birmingham and the University of Cambridge, found evidence of why NK cells adopt a dormant state when entering solid tumors. The team also determined that IL-15 can reverse this effect.
These findings point to possible ways of boosting immunotherapy regimens. The study appears in Nature Communications and the co-lead author is David Withers of the University of Birmingham.
“T cells have dominated thinking around cancer treatment and this was spurred on by the initial impacts of immune checkpoint blockade therapy which is clearly T cell mediated,” Withers tells Inside Precision Medicine. “There has been interest in CAR-NK cells as an alternative to CAR-T cells.” He also points out that IL-15 treatment is already being studied.
The challenge is to “wake up” the NK cells and see what effect that has.
“Up until now we have seen that NK cells have the innate capacity to slow cancers but often seem to lie dormant within tumor cells. [Through their studies] we have been able to specifically see what happens to natural killer cells after entering solid tumor environments—fwhich seemingly blunts their killer instinct,” says Withers.
Using tumor cells grown from mouse models, this team established that NK cells adopt a dormant state when entering solid tumors because of the loss of production of key immune effectors, including chemokines, cytokines, and granzymes. Further studies using human colon cancer cells confirmed that this loss of function happens in people too.
The team further tested whether the loss of function experienced by NK cells upon entering tumor environments could be reversed. Targeting the IL-15 pathway resulted in significantly more NK cell activity and in the mouse models and better tumor control.
“Natural killer cells are an exciting prospective field in the world of cancer treatment, using the body’s own immune system in the fight against cancer growth. Up until now though, we have seen that NK cells have the innate capacity to slow cancers but often seem to lie dormant within tumor cells,” says Withers.
He expects any potential for NK therapy would be in combination with immune checkpoint inhibitor treatments. He notes “It would make sense to push alongside T cells (e.g. in combination with ICB). It is logical that enhanced NK function can then feed into supporting the T cell response and so further pushing this through hitting the PD-1/PD-L1 pathway is obvious.”
What does this work mean for CAR-NK work? “Our data indicates that CAR-NK will lose function in the tumor, like normal NK do, so clever engineering approaches to counteract pathways that drive NK dysfunction is a logical approach to improving the treatment.”
He adds that, “I don’t think we fully yet understand the drivers of NK dysfunction – prostaglandins are one inhibitory mechanism, TGFβ another. But I think there are likely further mechanisms that also come into play.”
In a related study, which adds another piece to the puzzle, a team led by Withers and Menna Clatworthy, of the University of Cambridge, found that some dendritic cells (DCs) “get stuck” within cancers. DCs normally capture material from cancer cells and deliver this to lymph nodes where they stimulate anti-tumor immune responses. The team discovered that rather than trafficking to lymph nodes, some DCs stay in the tumor, where they become “exhausted.” This report was also published in Nature Communications,













