Talazoparib, a PARP inhibitor approved to treat breast cancer patients with mutations in the BRCA1 or BRCA2 genes, may also benefit people who have other genetic mutations, a recent study suggests
Researchers at University of Texas (UT) Southwestern reported in Nature Cancer that talazoparib shrank the tumors of breast cancer patients with mutations in the PALB2 gene. Patients with this mutation would not have previously qualified for treatment with the drug.
“These patients would otherwise have very limited treatment options,” said Joshua Gruber, MD, PhD, Assistant Professor of Internal Medicine at UT Southwestern. “This study expands the patient population that can benefit from PARP inhibitors.”
The team also found a potential biomarker for response.
“We used open-source algorithms to compute mutational signatures from the tumors in our study,” Gruber told Inside Precision Medicine. “This biomarker has been studied in many tumors before but our study is among the first to identify it in PALB2-associated tumors.”
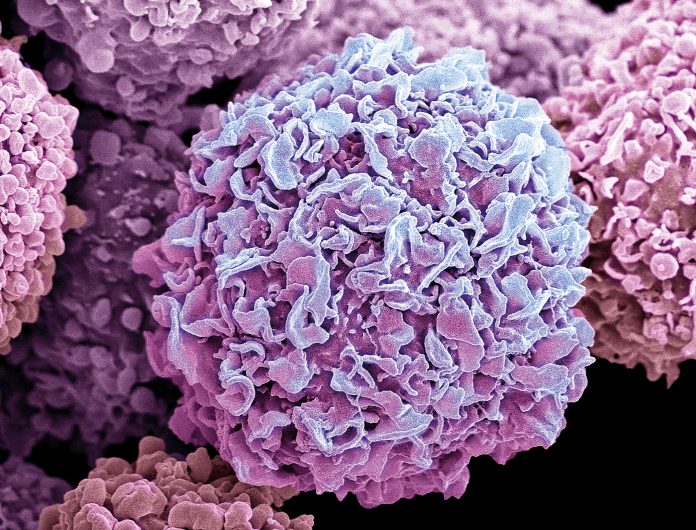
Like other PARP inhibitors, talazoparib works by blocking a DNA-repair protein. Without the ability to repair their DNA, cancer cells accumulate damage and eventually die. In cancers that have other defects in this process—including those with BRCA1/2 mutations—the drug is particularly effective, dealing a fatal second blow to the DNA repair machinery.
In a landmark 2018 study, researchers focused on advanced breast cancer patients with BRCA mutations—which account for 5% to 10% of all breast cancer cases—and found that talazoparib increased their survival time. The Food and Drug Administration approved the drug for that group, and follow-up studies have found that talazoparib also works for prostate and pancreatic cancer patients with BRCA mutations.
In this new Phase II trial, Gruber and colleagues tested the effectiveness of talazoparib in advanced cancer patients with less common gene mutations associated with DNA repair. Earlier data has suggested that more than 17% of all cancers have such mutations.
Twenty patients were enrolled in the trial at Stanford University, where Gruber previously served. Thirteen had breast cancer, three had pancreatic cancer, and four had other tumor types. The patients had mutations in eight DNA repair genes. On average, they took a daily talazoparib pill for 23.8 weeks.
Among all patients, the average survival time was 5.6 months, and 20% had at least partial shrinkage of tumors. Because this was a Phase II trial, there was not a control group to compare these data to, but the results were especially striking for patients with the PALB2 mutations: They survived 6.9 months on average, and all six patients (five with breast cancer, one with pancreatic cancer) had tumor shrinkage.
“We are still trying to understand why patients with mutations in homologous pathways repair genes develop some cancers but not others, that remains a very deep question in the field,” said Gruber.
The findings underscore the increasing importance of genetic testing to guide treatment for cancer patients, Gruber said. The team is planning a follow-up trial at UT Southwestern to further understand which patients gain the most benefit from talazoparib.
“Parp inhibitors are being explored in many tumor types,” said Gruber. “One interesting finding is that different mutations may behave differently in different tumor types. For example, ATM mutation was not a strong biomarker in our studies, but may be important in prostate cancers or other tumor types, which were not captured in our study.













