
By Pranali Pachika, Srijan Valasapalli, Phuong Ngo, and Goetz Kloecker
“Artificial intelligence” (AI) is the study and production of computing methods and models that replicate human intelligence in perception, speech recognition, decision making, and language processing.1 AI is utilized in oncology to improve cancer diagnosis, treatment planning, and patient outcomes by analyzing massive volumes of data from a variety of sources, including imaging scans, electronic health records, and genomic profiles.2,3 In 1956, John McCarthy coined the term “Artificial Intelligence” (AI) based on Alan Turing’s concept of machines mimicking human cognition.
Today, as a result of advances in computing power, AI integrates seamlessly into various aspects of our existence. Utilizing tools such as radiological images and electronic medical records, its recent foray into medicine has sped up patient care and improved diagnostic accuracy.4 McCulloch and Pitts presented a foundational model for neural processing back in the 1940s. Modern neural networks, which are primarily employed for data processing, draw inspiration from this concept.4 Despite advances in lung cancer detection, obstacles such as intergrader inconsistencies and incomplete characterization of imaging findings remained.
These obstacles prompted the development of more advanced AI-based systems that can improve performance and standardize inter-reader evaluations. Approaches based on deep learning paved the way for automated intricate image analysis, the identification of nuanced imaging details, and the establishment of standardized image evaluation methods.5 In the 1980s, the introduction of digital imaging techniques and advancements in computational architecture and storage reignited interest in computer aided detection (CAD) techniques. The initial success with AI in breast cancer detection paved the way for AI approaches to be used more extensively in diagnostic tasks such as tumor classification and cancer detection.6
In oncology, AI uses machine learning, deep learning, natural language processing, and computer vision. Machine learning involves creating algorithms and models that can learn from data and make predictions or judgments without programming.7 Oncologists use machine learning to examine massive clinical and genetic data sets to predict patient outcomes, treatment responses, and disease progression.8 Deep neural networks (DNNs) are a form of machine learning model capable of representing and classifying complex data patterns and relationships.
Multiple layers of interconnected nodes process information and extract increasingly abstract features from input data.9 Convolutional neural networks (CNNs) are a specific type of artificial neural networks that are extensively employed in the field of medical imaging. This is mostly attributed to their inherent capacity to effectively preserve and analyze spatial relationships within picture data. The feedforward network has been specifically built to handle spatial data through the application of filtering techniques, resulting in the generation of feature maps.10 Oncology uses CNNs for image analysis, diagnosis, and treatment planning.11
Deep learning uses DNNs to learn from complicated high-dimensional data such as medical imaging and genomic profiles. Deep learning is used in oncology to analyze computed tomography (CT) scans and other images to detect tiny traits and patterns that humans may miss.12 Natural language processing extracts patient history, diagnostic, and treatment information from electronic health records and other clinical documents in oncology.13 Computer vision algorithms and models analyze and interpret visual data such as medical photographs and videos. Computer vision is used in oncology to evaluate medical pictures such as CT and magnetic resonance imaging (MRI) scans to discover cancer-related traits and patterns.14,15
Lung cancer is one of the leading causes of cancer-related deaths in both men and women and requires highly individualized treatment.16 The detection of pulmonary nodules, the staging of cancer, and the evaluation of tumor progression are all complex processes best served by a multidisciplinary approach. Currently there are a limited number of quantitative measurements for pulmonary lesions, including CT-based largest diameter of nodules detected incidentally or in a screening setting using the Fleischner Society17 or Lung Imaging Reporting and Data System (Lung-RADS)18 guidelines, SUV-derived metrics from positron emission tomography (PET), and percentage enhancement of lesions on MRI.19
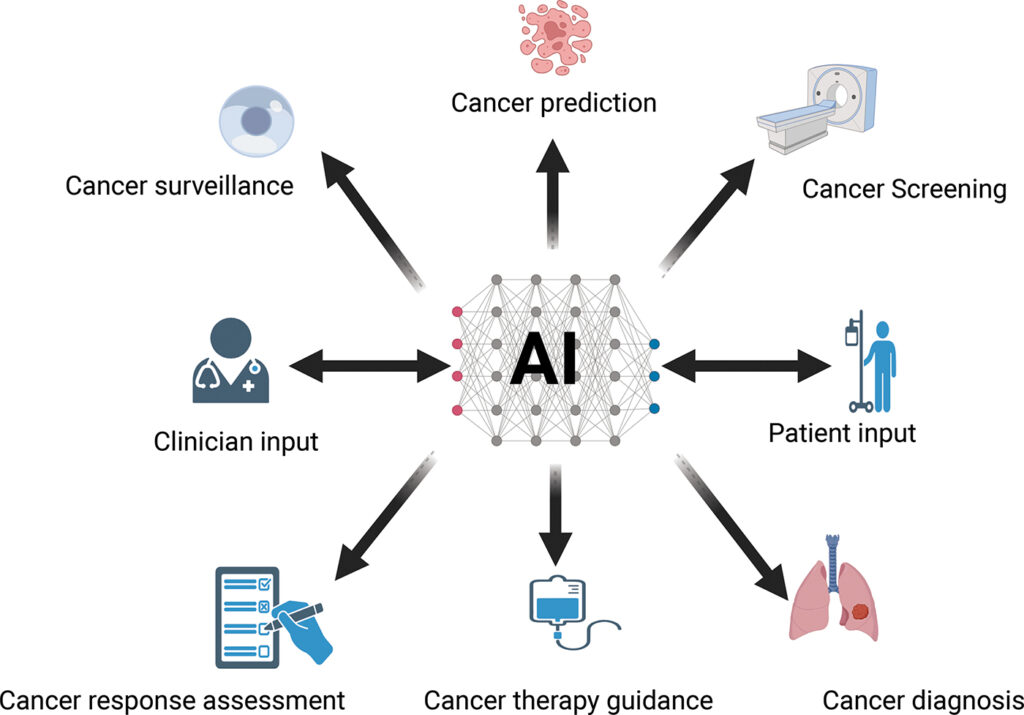
AI tools such as machine learning and deep learning are used at every step of treating lung cancer, from diagnosing the disease to predicting how the treatment will work. The FDA has approved multiple AI applications for lung cancer.20 Figure 1 depicts the workflow of how AI is assisting in lung cancer management.
To read this article in its entirety please visit the AI in Precision Oncology article.
Pranali Pachika ([email protected]), Phuong Ngo, and Goetz Kloecker are from the Department of Hematology-Oncology, University of Louisville. Srijan Valasapalli is from the Department of Hematology-Oncology, East Carolina University.
AI in Precision Oncology, published by Mary Ann Liebert, Inc., is the only peer-reviewed research journal dedicated to the advancement of artificial intelligence applications in clinical and precision oncology. The above article was first published in the February 2024 issue.












