Offering clinical whole-genome sequencing (WGS) to every child with suspected cancer changes the treatment plan in around one in 14 patients, suggests an analysis of data from two English hospitals where the test is routinely offered.
Senior author, professor Sam Behjati, from the Wellcome Sanger Institute, Cambridge University Hospitals, and the University of Cambridge said the findings “clearly justify using whole genome sequencing for assessing [pediatric] cancers to enable us to make highly patient-specific treatment plans.”
He explained that, in England, every child with suspected cancer can access WGS free of charge through the National Health Service, more specifically through the Genomic Medicine Service, but it was unknown whether offering this test can provide clinical benefits beyond standard-of-care (SOC) molecular tests.
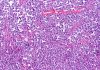
To investigate, Behjati and team examined 282 tumors from 281 children treated at Great Ormond Street Hospital in London and Cambridge University Hospitals. Both centers systematically deployed WGS for consecutive children with leukemia and solid tumors, respectively, with near-universal uptake (289 out of 291) by children and/or their legal guardians.
They compared WGS data to the results of 738 SOC tumor and germline molecular tests carried out across the whole cohort, including fluorescence in situ hybridization, mutation-specific immunohistochemistry, targeted DNA sequencing targeted RNA sequencing for gene fusion detection, and karyotyping.
The authors reported in Nature Medicine that “WGS faithfully reproduced findings (including absence of disease-relevant features) from all these assays.”
This suggests that “centralized WGS and variant calling could, in principle, replace all molecular assays deployed in this cohort,” they remarked.
It took a median 17 days for clinicians to receive the WGS results, which were interpreted by clinical scientists at the Genomic Medicine Center. The researchers described this as “comparably fast” and suggest it could accelerate definitive therapy, “which is likely to improve outcomes by reducing pretreatment morbidity and mortality.”
WGS provided additional diagnostic, risk, and therapeutic information, as well as details of previously unknown genetic features in 108 instances for 83 (29%) cases.
In addition, Behjati and colleagues determined that WGS provided clinical benefit in 80 instances across 69 (24%) cases by aiding diagnoses through accelerating expected findings or providing additional diagnostic information (14%); providing therapeutic opportunities such as variants targetable through existing drugs (7%); and changing management (7%).
Examples of management changes included the identification of a breast cancer-predisposing germline variant in a girl with a thoracic neuroblastoma. The variant had not been routinely tested for because it was deemed irrelevant to neuroblastoma, yet the discovery led to a change in her radiotherapy field to avoid exposure of breast buds.
Another case involved the discovery of a gene fusion in a child with B cell acute lymphoblastic leukemia that is rarely detected by SOC assays. Normally, the child would have been offered intensified therapy due to residual disease but the gene fusion that was discovered confers good overall prognosis, which enabled clinicians not to escalate therapy.
Behjati believes that WGS could eventually replace the multiple molecular tests currently used when a child is undergoing investigations for cancer.
“I suspect that ultimately it will be more cost-efficient to have a single, relatively expensive test rather than running lots of cheaper tests that require a multitude of equipment, pipelines, and staff,” he told Inside Precision Medicine.