Research led by the Chinese University of Hong Kong shows that changes in the gut microbiome occur before the development of eczema in young children.
As reported in the journal mSystems, the researchers noted that the genera Clostridium sensu stricto 1 and Finegoldia were present in higher amounts before eczema onset in the gut of children who developed eczema compared with those who did not, whereas Bacteroides levels were lower.
“The problem of eczema is increasing, and our study shows it could be a result of unwanted changes in the gut bacterial content. The first year of life could be a critical period to restore the gut bacteria to a more desirable composition,” said lead author Paul Chan, professor of microbiology at the Chinese University of Hong Kong, China, in a press statement.
The gut microbiome and its link to the developing immune system is a hot research topic at the moment and early microbiome abnormalities have been linked to inflammatory and allergic childhood disorders in other recent research.
In this study, Chan and colleagues recruited 112 Chinese mother-child pairs before birth and took stool samples at nine different time points between birth and three years of age. The children were born between September 2017 and April 2018, 51% were male and 76% had a vaginal delivery. In addition, 51% of the mothers received antibiotics during the birth period. Just under a quarter had been solely breastfed at six months old and 57% were given solid food before 6 months.
At six and 12 months of age 43% and 30% of the infants had physician diagnosed eczema, respectively, most cases of which (more than 70%) were mild or moderate according to the official scoring atopic dermatitis (SCORAD) and objective scoring atopic dermatitis (oSCORAD) scores.
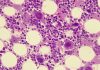
Using 16S rRNA gene sequencing to characterize the microbiome of these children at the different time points, the researchers discovered significant differences in microbiome composition between children who developed eczema in the first few years of life and those who did not.
The team showed Bacteroides was depleted and Clostridium sensu stricto 1 and Finegoldia enriched in children who had developed eczema at one years old compared with levels in the control children. When the researchers just looked at the microbiome of babies born by C-section, they had a similar microbiome composition to the children that developed eczema.
Factors that appeared to significantly influence early microbiome composition up to 12 months of age included: mode of delivery (vaginal vs C-section), feeding mode, and maternal intrapartum antibiotic treatment.
“Our study found that the gut bacterial content of babies changes drastically over the first three years of life,” said Chan. “We observed characteristic changes in the gut bacterial content before the babies present with eczema. Remarkably, those bacterial changes were also observed in babies delivered by C-section. Nevertheless, the link between C-section and eczema requires further studies to verify.”
The researchers now plan to carry out further studies to confirm their results and assess if early microbiome-based treatments could help prevent eczema developing in vulnerable children.