New research out of Dana-Farber, the Broad, and Harvard Medical School improves our ability to forecast the alloreactivity of hematopoietic cell transplants (HCTs), which could significantly improve patient outcomes in precision immuno-oncology and allogeneic HCT (allo-HCT) and lead to fewer post-transplant diseases.
The cause of allo-HCT-related disease
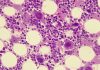
The leading cause of alloreactivity in HCT is the immune system’s reaction to minor histocompatibility antigens (mHAgs). These polymorphic peptides can cause immune responses between donors and transplant recipients, even if they are HLA-matched. In the same way that tumor neoantigens are recognized as foreign by donor T cells, mHAgs lack central tolerance, making them highly immunogenic. In contrast to tumor-specific antigens, mHAgs manifest not as somatic events but as germline traits encoded by polymorphic genes.
There are two sides to the alloreactive coin when it comes to allo-HCT. On the one hand, the most detrimental immune-related complication following allo-HCT, graft-versus-host disease (GvHD), can be attributed to a donor-derived immune response directed against mHAgs. This response may be broadly expressed across tissues or specifically in GvHD-affected tissues. On the other hand, the curative graft-versus-leukemia (GvL) effect can be conceptualized as the result of productive donor immune responses against mHAgs expressed on hematopoietic cells, including but not limited to epitopes with hematopoietic tissue restriction.
The molecular characterization of donor-recipient pairs can facilitate the design of personalized post-HCT treatments to minimize this highly morbid condition. This includes incorporating additional immunosuppressive therapies introduced early for high-risk patients or reduced-intensity approaches in low-risk settings.
Personalizing mHAg prediction in allo-HCT
The study, published in Nature Biotechnology, was based on developing a comprehensive analytic framework to predict candidate mHAgs expressed in organs frequently targeted by GvHD or hematopoietic cells. Whole-exome sequencing (WES) was used to find mHAgs, which helped researchers predict alloreactivity and prognostication risk. Single-cell RNA sequencing (scRNA-seq) was added to find possible mHAgs that would be safe to use as therapeutic targets.
Application of this pipeline to 220 HLA-matched allo-HCT donor-recipient pairs demonstrated that total and organ-specific mHAg load could independently predict the occurrence of acute GvHD and chronic pulmonary GvHD, respectively. They also identified promising GvL targets for preventing or treating post-transplant disease recurrence, confirmed in a validation cohort of 58 donor-recipient pairs.
Future studies can use this pipeline’s capacity to effectively process massive patient datasets to hone the algorithm for more sensitive prognostication and HCT response prediction. Allo-HCT study populations from various ethnic backgrounds, especially those from Asia or Africa, could be analyzed as part of these datasets. This would increase the number of usable GvL mHAgs and population coverage.