A new study by Rutgers University researchers suggests that two genes expressed in the intestinal cells that line the inside of the colon may also be involved in cancer development.
Recent studies have shown that intestinal stem cells can increase in animals on a high fat “Western” diet, potentially explaining an elevated cancer risk from such a diet. Diet being able to control cell proliferation is an interesting research development, particularly the convergence of dietary factors and dysregulated gene signaling driving malignant transformations and promoting an adenoma-to-adenocarcinoma progression.
This new study suggests a novel connection between HNF4A and HNF4G genes, diet and cancer. Genetic expression of HNF4 has previously been shown by to be heavily influenced by the gut microbiota, which in turn can influence a multitude of intestinal disorders.
Non-host gene regulation was further explored in this study by using a high fat diet to test how these genes work, and the researchers discovered they help co-regulate stem cell proliferation, as well as help intestine cells burn dietary fat. This was done by isolating cells from knockout and control mice and observing intestine stem cell proliferation under conditions of high fat and control. Mice that had both HNF4A and HNF4G knocked out were unable to have their stem cells proliferate under high fat conditions.
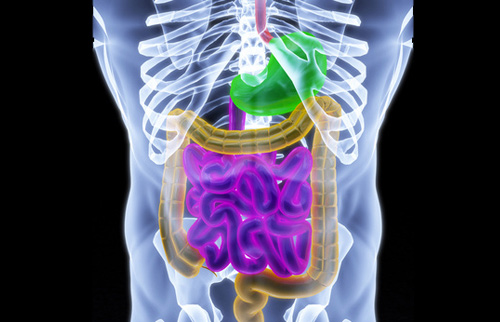
Intestinal stem cells undergo constant renewal and fuel the continuous turnover of the lining of the intestine. People naturally lose millions of intestinal cells daily, much like they lose skin cells. If this rate of replication is not closely controlled, it can quickly lead to malignancy. Lack of proliferation can be very problematic for the colon and damaging to lower layers of cells.
“This [research] is important because scientists have shown that when there’s too much dietary fat in the intestine, stem cell numbers increase, boosting susceptibility to colon cancer,” said senior author Michael Verzi, an associate professor in the Department of Genetics in the School of Arts and Sciences at Rutgers University–New Brunswick.
Rutgers scientists believe HNF4A and HNF4G help stem cells burn fat, providing them energy. By linking gene activation, cell replication number, diet and cancer risk, scientists might be able to better understand the cancer development process in high risk patients. Going forward, the researchers plan to continue studying whether these two genes alter stem cell numbers and cancer risk alongside a high fat diet, said Verzi.
Colorectal cancer (of the colon or rectum) is the third most common cancer diagnosed in both men and women in the United States. According to the American Cancer Society, over 100,000 Americans will be diagnosed with colon cancer this year. This cancer is also the second most deadliest in the United States, but due to a combination of increased screening and heightened awareness the death rate has been dropping. However, in patients under the age of 55, the death rate of colon cancer has increased each year by 1% since 2007. Approximately 50,000 colon cancer patients are expected to die in 2019.













