A nanogel-based carrier that delivers a drug exclusively to the liver effectively reversed obesity in mice.
“The treated mice completely lost their gained weight, and we did not see any untoward side effects,” said senior author S. Thai Thayumanavan, professor of chemistry and biomedical engineering, and director of the Center for Bioactive Delivery at the UMass Institute for Applied Life Sciences (IALS).
“We really wanted to find out the factors that got affected,” Thayumanavan said. “We found that we are activating the reverse cholesterol transport pathway. We believe that activation of fat oxidation and an increase in metabolic rate are causing the loss in weight, but more work needs to be done to prove that point.”
The team’s findings were published last week in the PNAS Nexus. Ruiling Wu, is the paper’s lead author.
Thyromimetics, or drugs that mimic synthetic thyroid hormone, have been considered as a way to tackle obesity, type 2 diabetes, high cholesterol, metabolic dysfunction-associated steatohepatitis (MASH), and other metabolic conditions. Thayumanavan and his team looked at one such thyromimetic.
“We realized we needed to deliver this drug selectively to the liver because if it goes to other places, it could cause complications,” he said. In addition to side effects, taking the drug systemically was expected to dilute its effectiveness, which was confirmed in the study.
“Considering 100 million Americans have obesity and related cardiometabolic disorders, we became pretty excited about this work,” he said.
Efforts to translate these findings to humans are being pursued by a start-up company Cyta Therapeutics, which was founded at IALS. The company’s lead product, Cyta-001, is described as, “a liver-targeted IntelliGel in which a potent thyromimetic drug has been non-covalently encapsulated inside the polymer.”
“There is a significant amount of development work to be conducted between mice and humans,” Thayumanavan said, “but we are hoping it will eventually become a drug.”
One of the IALS’s primary goals is figuring out how to get the right drug to the right place in the body by creating novel delivery platforms for small and large molecules.
In this study, Thayumanavan’s team fed a group of mice a high-fat, high-sugar, high-cholesterol diet for 10 weeks, doubling their weight. A control group of mice were fed a healthy diet.
“We came up with a very simple approach, using our unique invention – nanogels that we can direct selectively to different targets, which we call IntelliGels,” Thayumanavan said. “They were custom-designed for hepatocyte delivery in the liver.”
The obese mice were given the drug daily, packaged inside the nanogel and delivered to the mice via intraperitoneal (IP) injection.
Once the nanogel carrier is inside the hepatocyte cells, glutathione in the cells breaks down bonds in the nanogel, releasing the drug. The drug then activates thyroid hormone beta receptor, leading to systemic lipid lowering, increased bile acid synthesis and fat oxidation.
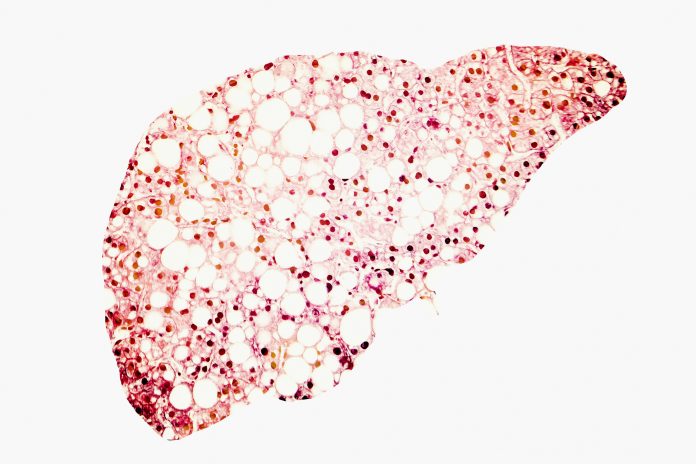
After five weeks of treatment, the mice returned to a normal weight—even as their high-fat diet continued. The mice also saw their cholesterol levels drop and their liver inflammation resolve.
Now that the mechanism is better understood, the paper notes, “the drug-encapsulated nanogels open up the possibility for nanoparticle-mediated pharmaceutical strategies for other liver-based diseases.”













